Clinical Research & Literature — Respiratory
Inhalation Devices
The pulmonary route of delivering drugs and biopharmaceuticals has proved to be effective locally and systemically.

Clinical Research & Literature — Respiratory
Inhalation Devices
The pulmonary route of delivering drugs and biopharmaceuticals has proved to be effective locally and systemically.
Inhalation drug delivery devices cover many different types: pressurized metered dose inhalers (pMDIs), breath-activated inhalers (such as dry powder inhalers (DPIs)), emerging novel delivery systems and nebulizers.
Inhalation drug delivery devices: technology update¹
The pulmonary route of delivering drugs and biopharmaceuticals has proved to be effective locally and systemically.
A successful pulmonary administration requires a harmonic interaction between the drug formulation, the inhaler device, and the patient. One of the biggest problems concerning the lack of desired effect comes due to an incorrect use of the device. This review summarizes the advantages and limitations of the most used inhaler devices.
Choosing the right inhaler for your asthma or COPD patient²
Not one device suits all patients. Challenges can range from difficulties related to lung disease severity and pulmonary function, to physical considerations, including manual dexterity and comorbidities such as arthritis. Furthermore, patient engagement and satisfaction are also crucial factors to consider. A tailored and personalized approach is highly recommended to achieve improved disease outcomes. This paper discusses the aspects for consideration with nebulizers, pressurized metered-dose inhalers, dry powder inhalers and the soft mist inhaler.
Considerations for managing chronic obstructive pulmonary disease in the elderly³
Nebulizers should be considered for patients unable to use handheld inhalers properly. Once set up, they are easier for patients to use than handheld devices as they only require normal tidal respiration for effective drug delivery. Most patients in the emergency department, needing inhaler medication, are treated with a nebulizer. They are also effective for maintenance dosing in populations who cannot use other devices, such as patients with cognitive, neuromuscular, or ventilatory impairments. 56% of the patients using nebulizers do so because of physical and cognitive disabilities.
Systematic Review of Errors in Inhaler Use – Has patient technique improved over time?⁴
Incorrect inhaler technique occurs frequent and has not improved over the past 40 years. Data from 144 articles show that the most frequent MDI errors were in coordination (45%; 95% CI, 41%-49%), speed and/or depth of inspiration (44%; 40%-47%), and no post inhalation breath-hold (46%; 42%-49%). Frequent DPI errors were incorrect preparation in 29% (26%-33%), no full expiration before inhalation in 46% (42%-50%), and no post inhalation breath-hold in 37% (33%-40%). The overall prevalence of correct technique was 31% (28%-35%); of acceptable, 41% (36%-47%); and of poor, 31% (27%-36%).
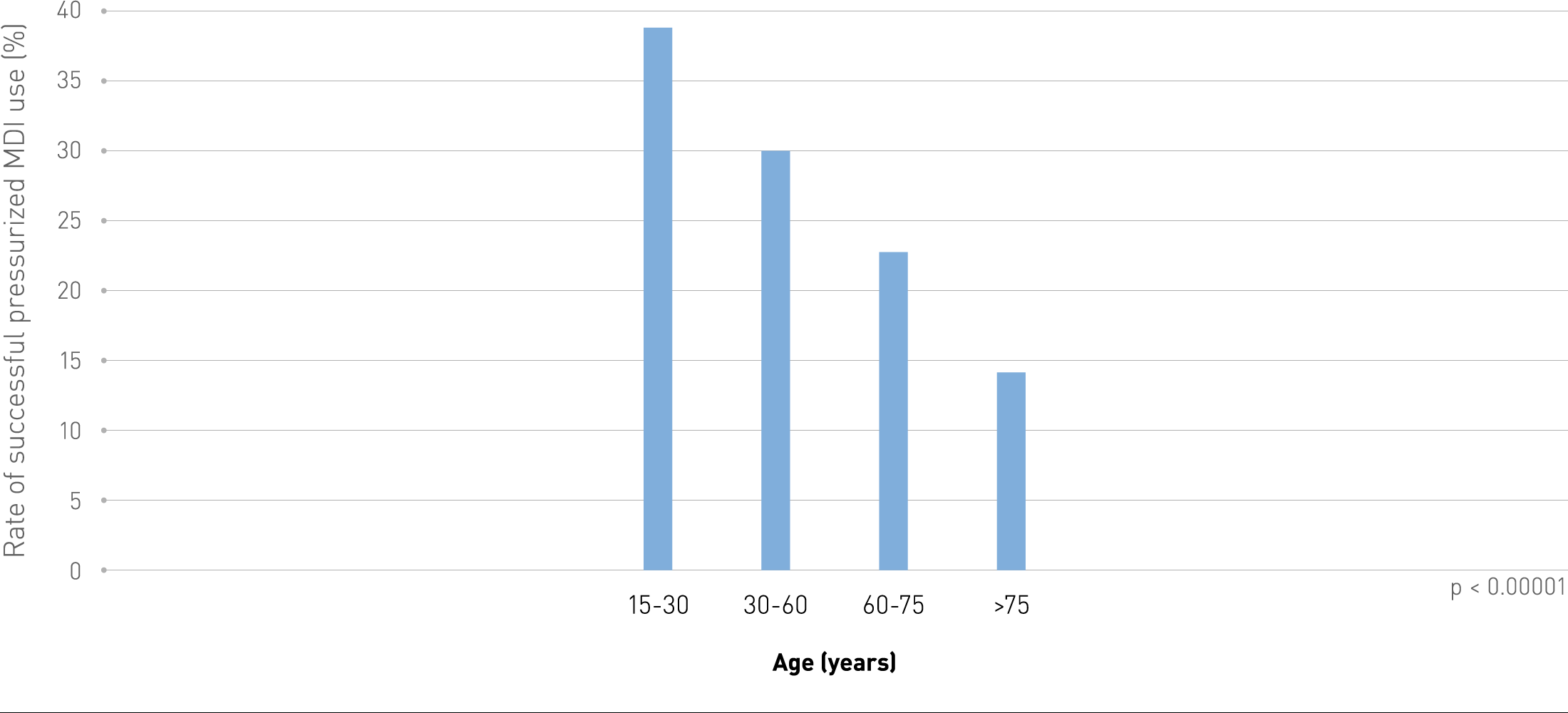
Decrease in frequency of successful use of pressurized MDI with patient age.
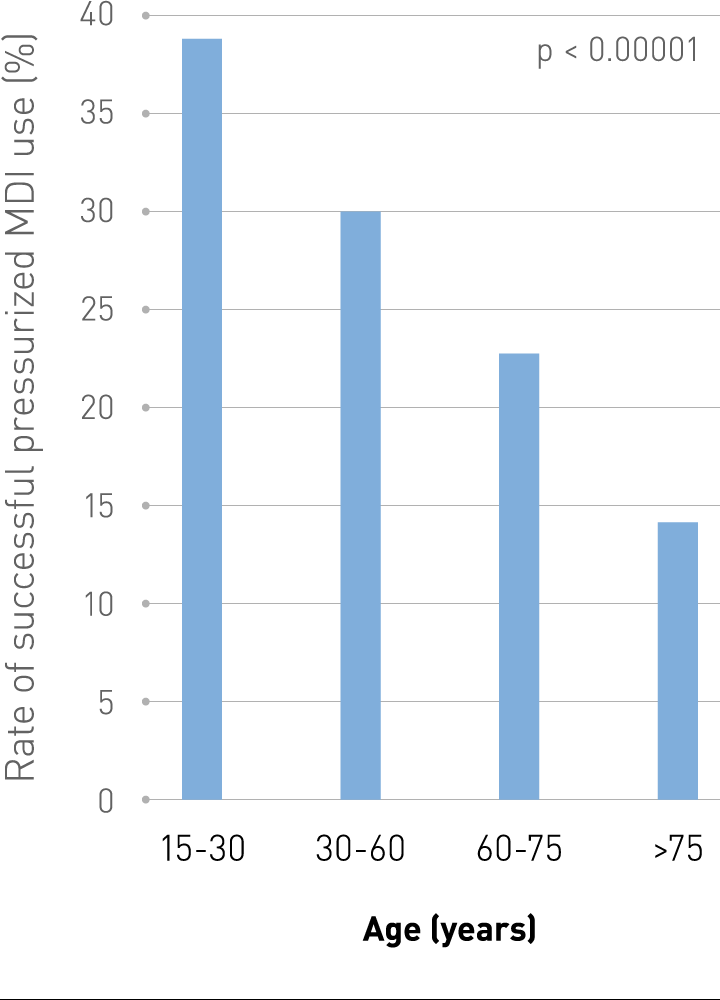
Decrease in frequency of successful use of pressurized MDI with patient age.
Spacer devices for inhaled therapy: why use them, and how?⁵
This extensive review of the literature is about the rationale for using a spaced/valved holding chamber (VHC) to deliver inhaled therapy from a pressurized metered-dose inhaler. Discussing on how the properties of individual devices may vary according to their physical characteristics and materials – and the potential risks and benefits. One of the important factors mentioned in this article are the two material types of manufacture (Plastic Polycarbonate Polymer and Metallic (steel or aluminium) Some Plastics) and the consequences of it on the delivery of the aerosol dosage. Patients should know how to properly use it, how to keep it clean and how to keep an eye out for faults.
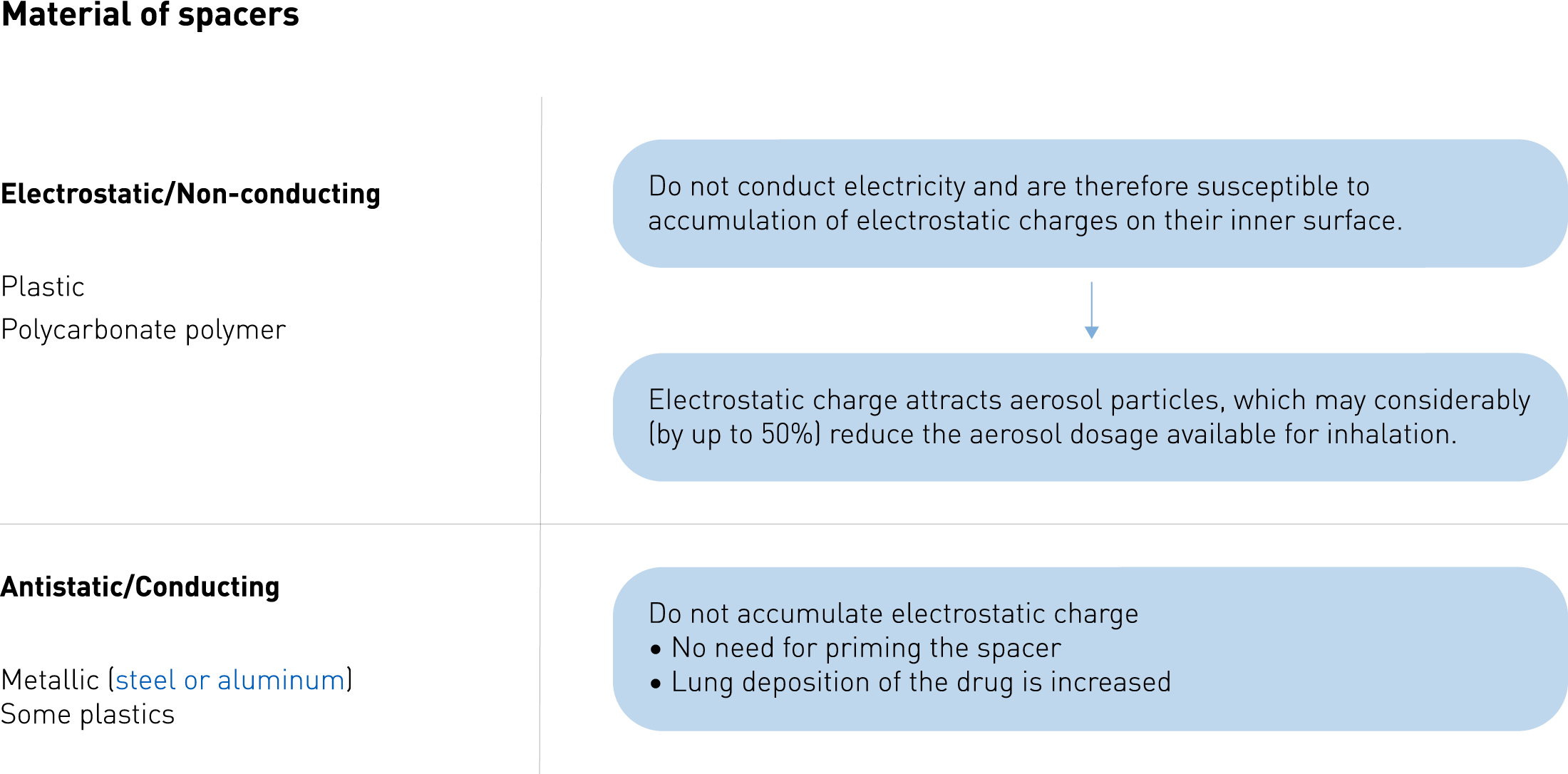
Materials of spacers (Plastic Polycarbonate Polymer and Metalic (Steel or aluminuim) Some Plastics.
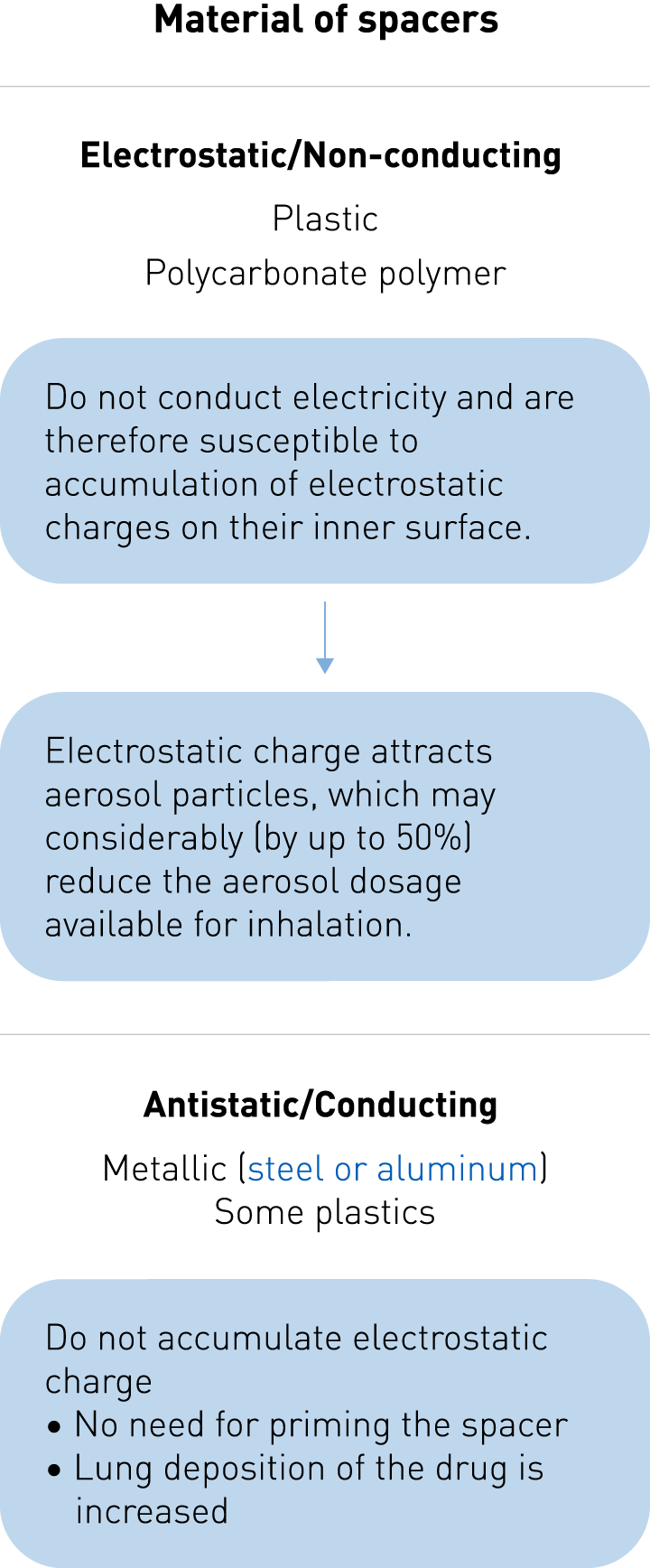
Materials of spacers (Plastic Polycarbonate Polymer and Metalic (Steel or aluminuim) Some Plastics.
Main takeaways
Inhalation Devices
A successful pulmonary administration requires a harmonic interaction between the drug formulation, the inhaler device, and the patient.¹
A tailored and personalized approach is highly recommended to achieve improved disease outcomes.²
Nebulizers should be considered for patients unable to use handheld inhalers properly.³
Incorrect inhaler technique occurs frequent and has not improved. The overall prevalence of correct technique was 31% (28%-35%); of acceptable, 41% (36%-47%); and of poor, 31% (27%-36%).⁴
The two material types of pMDIs (Plastic Polycarbonate Polymer and Metallic (steel or aluminium) Some plastics) have consequences on the delivery of the aerosol dosage.⁵



