Clinical Research & Literature — Respiratory
Chronic Obstructive Pulmonary Disease (COPD)
Early diagnosis and early treatment are critical for slowing down the progression.

Clinical Research & Literature — Respiratory
Chronic Obstructive Pulmonary Disease (COPD)
Early diagnosis and early treatment are critical for slowing down the progression.
Chronic bronchitis & Emphysema
COPD includes chronic bronchitis and emphysema and is a common, progressive disease. It is marked by persistent respiratory symptoms and airflow limitations due to airway and/or alveolar abnormalities. All of this is mainly caused by significant exposure to noxious particles or gases. It is the third leading cause of death worldwide, with 3.23 million deaths in 2019. Over 80% of these deaths occurred in low-and middle-income countries. There is no cure for COPD, but early diagnosis and early treatment are critical for slowing down the progression.¹
Summarizing the 2021 Updated GOLD Guidelines for COPD²
Early detection and appropriate treatment and management of COPD can lower morbidity and perhaps even mortality. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines summarize and evaluate available evidence with the aim of assisting healthcare professionals in selecting the best strategy. This review provides an overview of the GOLD 2021 report – Diagnoses, Assessment and Classification.
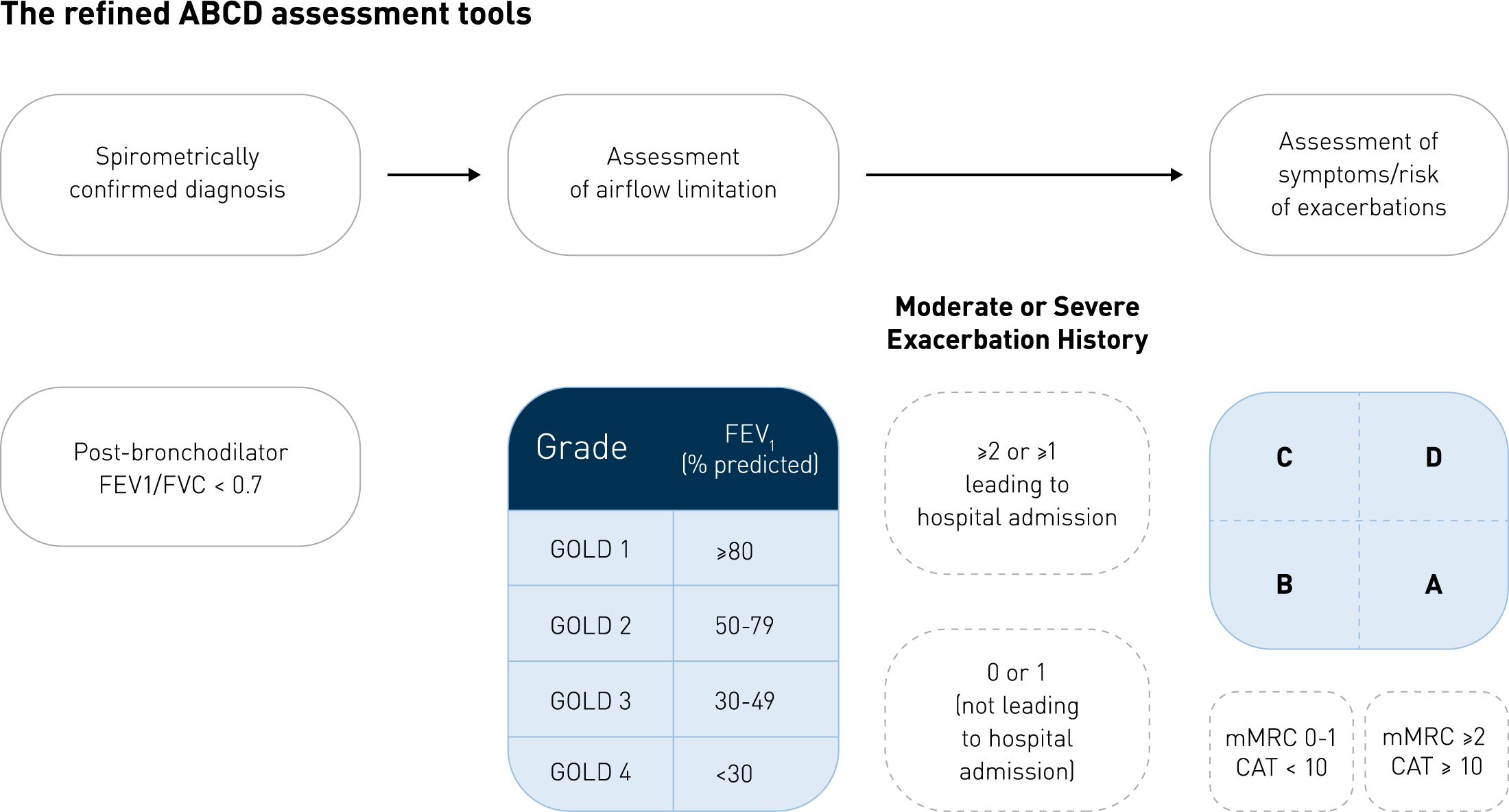
Assessment tool of COPD – GOLD group classification
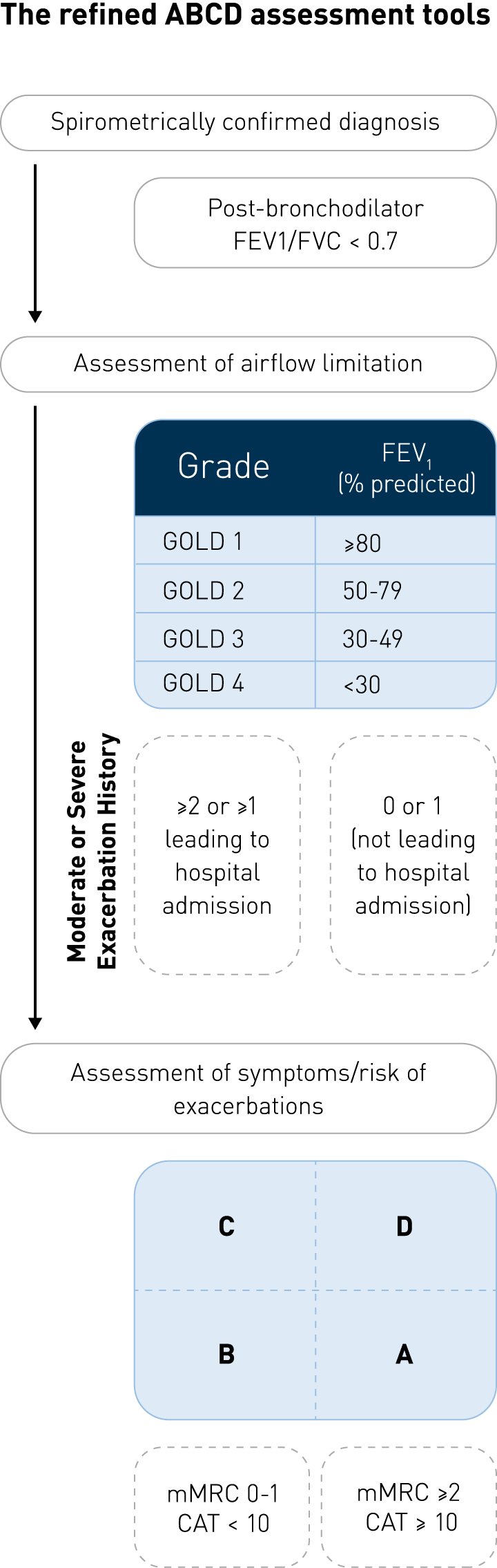
Assessment tool of COPD – GOLD group classification
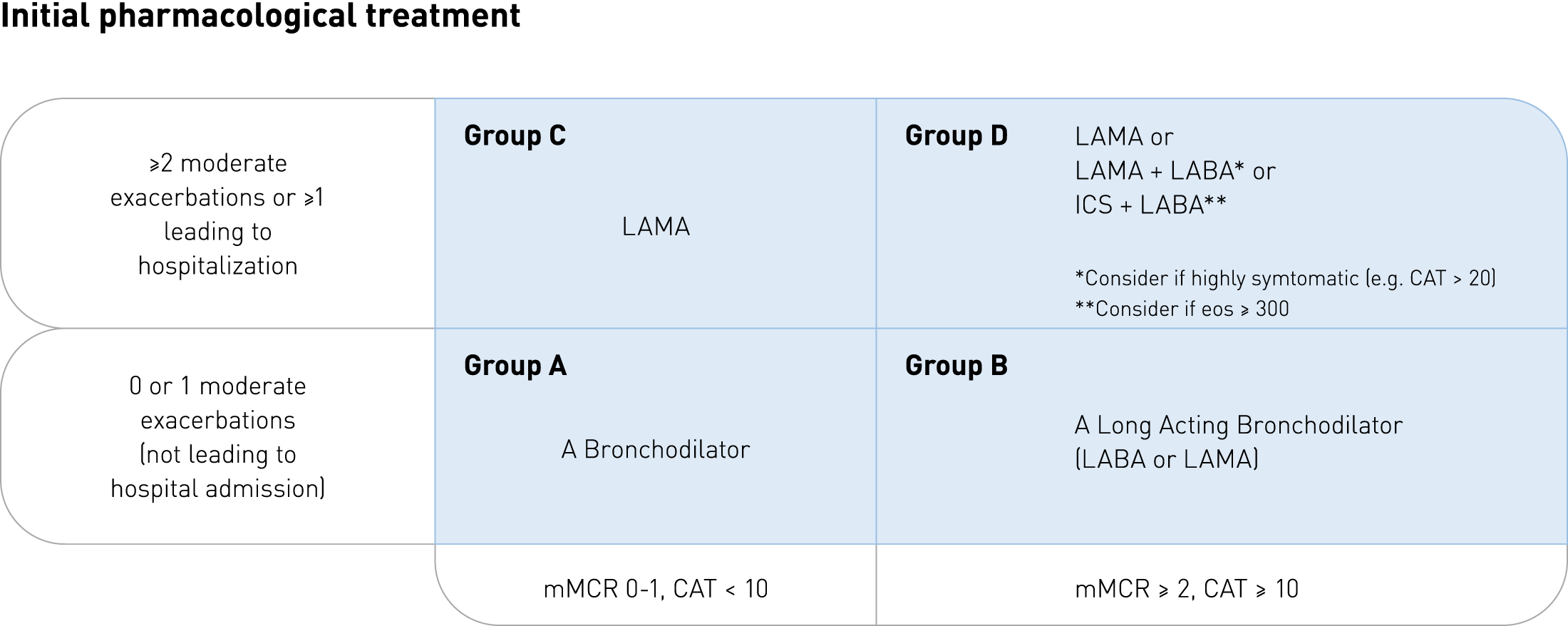
Follow-up recommendations
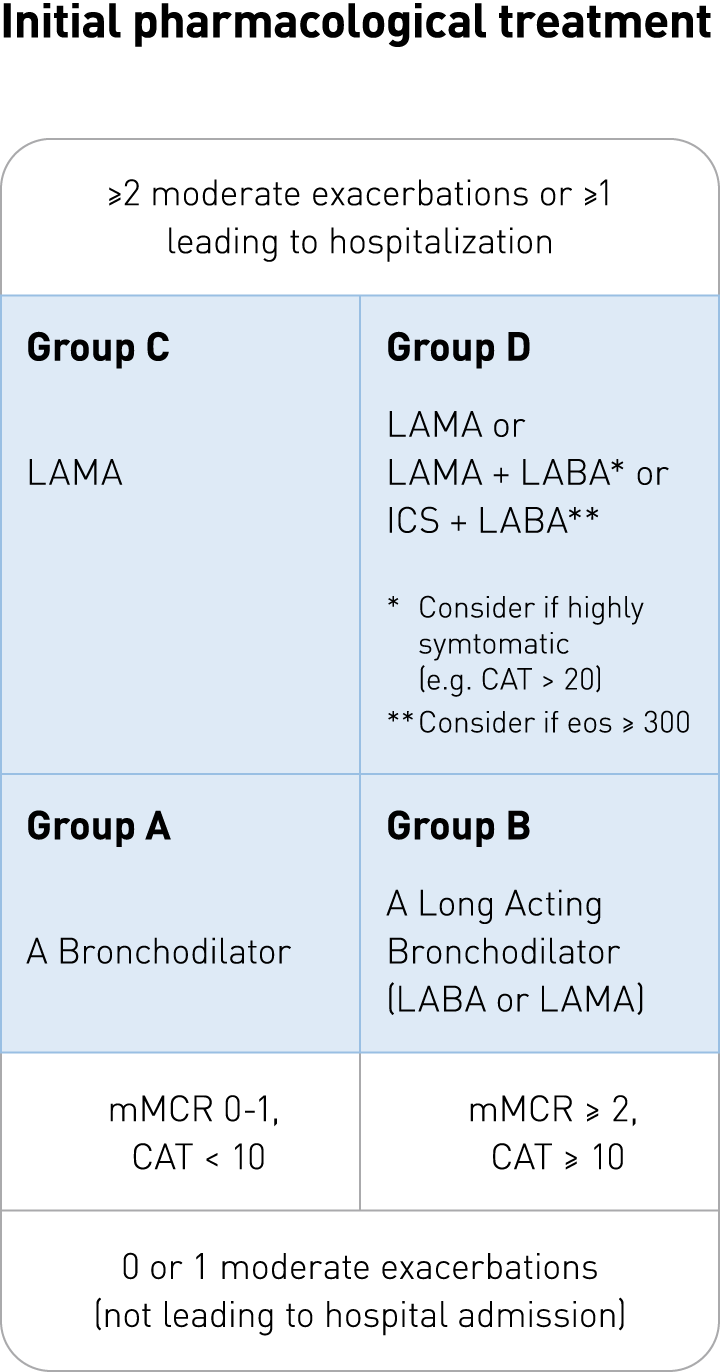
Follow-up recommendations
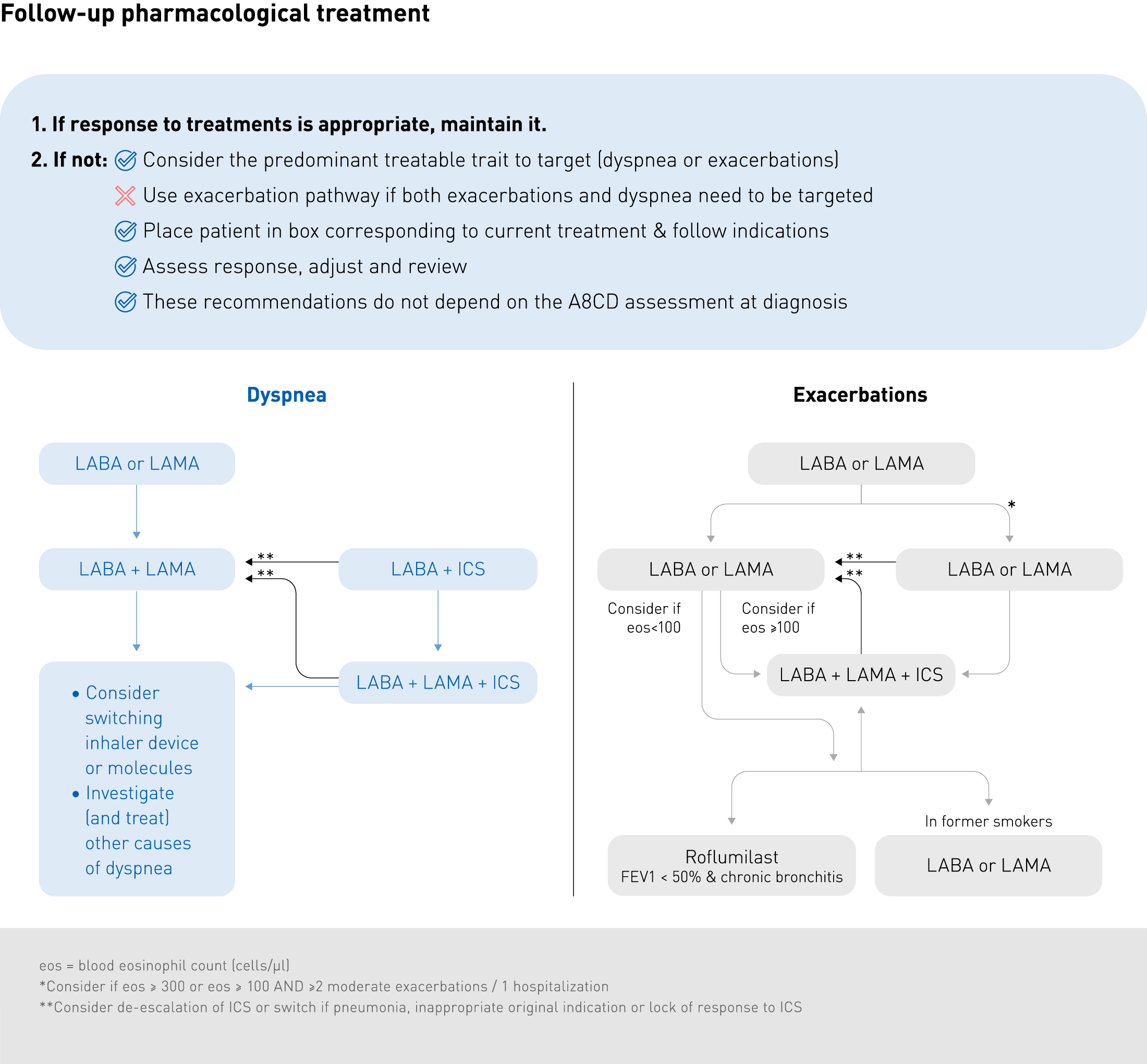
Follow-up recommendations
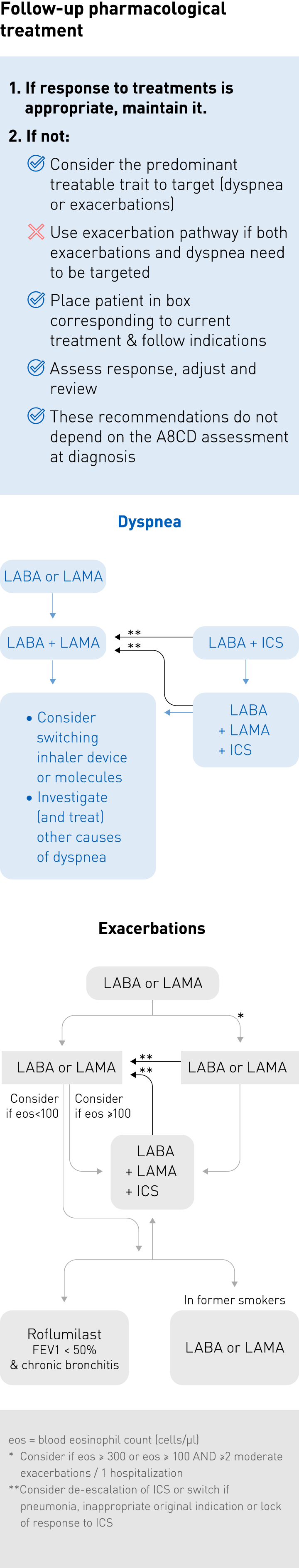
Follow-up recommendations
Pulmonary Disease³
Around 300 million people worldwide are affected by COPD, which results in approximately 64 million disability-adjusted life years. Occupational exposures account for 14% of the overall COPD burden. Populations living in rural areas have a higher risk for COPD than populations living in urban areas. Further analysis of the epidemiology of COPD can be read in this paper.
Air pollution, lung function and COPD: results from the population – based UK Biobank study⁴
Ambient air pollution increases the risk of respiratory mortality. The aim of this study was to evaluate whether ambient air pollution is associated with lung function and COPD. Effect modification was investigated for sex, age, obesity, smoking status, household income, asthma status and occupations previously linked to COPD. Higher exposures to each pollutant were significantly associated with lower lung function. Stronger lung function associations were seen for males, lower income households, “at risk” occupations. Higher COPD associations were seen for obese, lower income and non-asthmatic participants. Furthermore, ambient air pollution was associated with lower lung function and increased COPD prevalence.
Exercise Capacity in Chronic Obstructive Pulmonary Disease: Mechanisms of Limitation⁵
Patients with COPD are often caught in a downward spiral, going from expiratory flow limitation to poor quality of life and invalidity. Within this spiral, exercise tolerance represents an important intermediate outcome. As stated by the GOLD initiative, improvement in exercise tolerance is a key goal of COPD treatment. However, this objective can only be achieved by a comprehensive understanding of the mechanism of exercise limitation in COPD patients. This paper reviews the mechanisms and discusses their relative contribution to exercise intolerance.
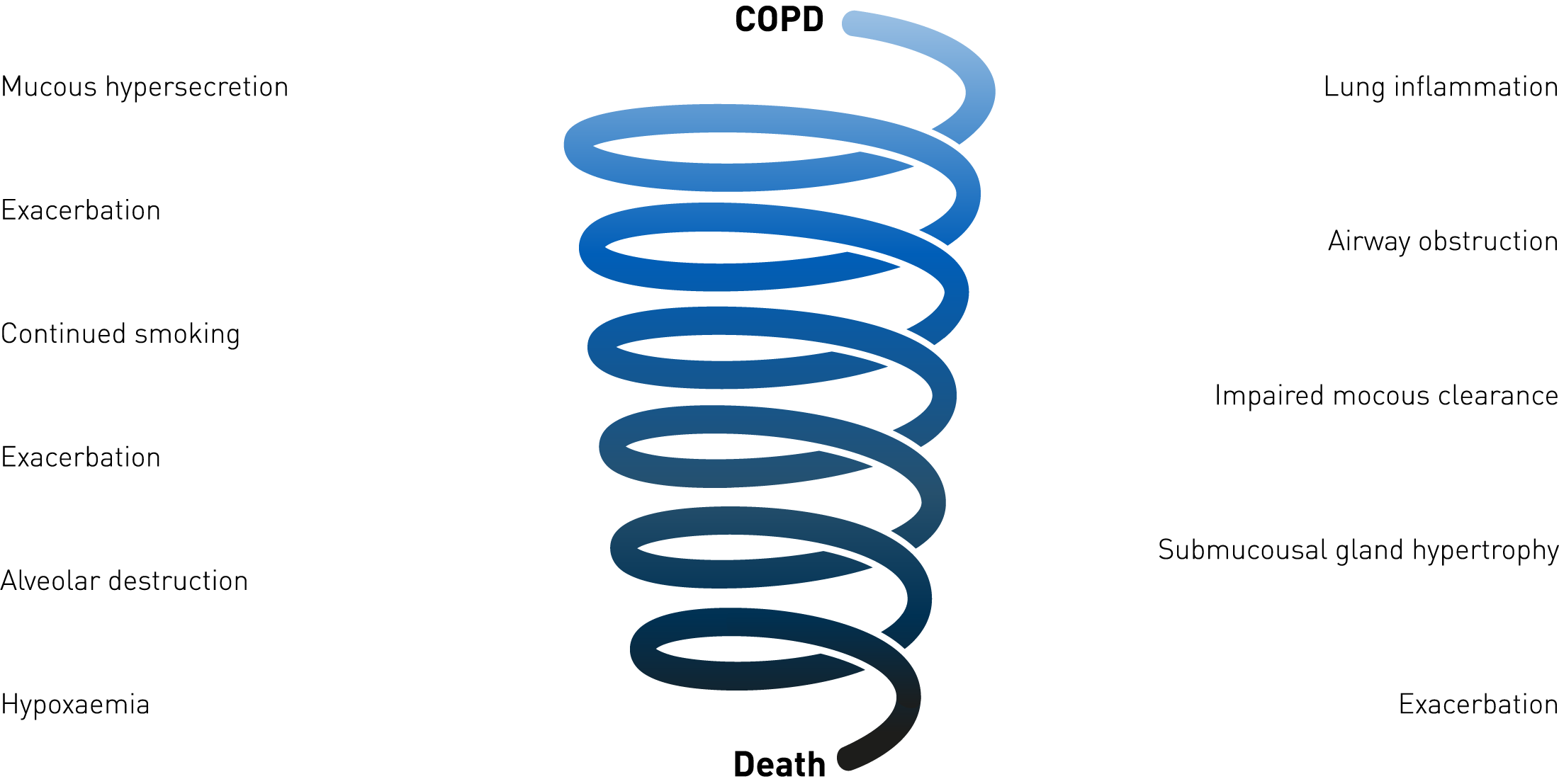
The downward spiral in COPD
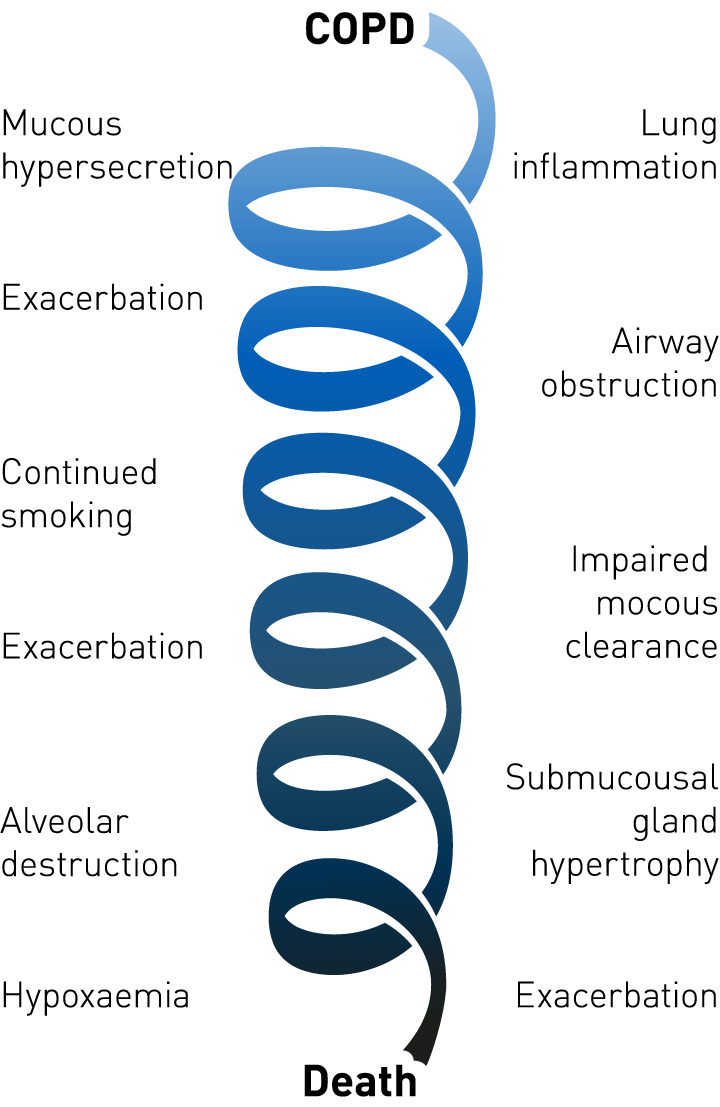
The downward spiral in COPD
Exacerbation
Many COPD patients live with the constant threat of an exacerbation. An exacerbation or lung attack is an acute worsening of symptoms which can lead to permanent loss of lung function and increased risk of mortality. Patients often experience it, but do not always report it. Consequently, they are left under-treated.
Patient’s perception of exacerbation of COPD – the PERCEIVE study⁶
This study evaluated the perceptions of patients with COPD, their exacerbations, and expectations of treatment. From 83.592 households screened, 1100 subjects with symptoms compatible with COPD were identified. The most frequent symptom was shortness of breath (78%) and the most frequent complaint was that due to their COPD, they could not complete their activities (54%). Of the individuals, 17% were afraid that their COPD would cripple or kill them. Exacerbations generated a mean of 5.1 medical visits/year, with around 10.5 days as the duration of having exacerbation symptoms. 55% of patients said that quicker symptom relief was the most desired requirement for treatment.
Negative impacts of unreported COPD exacerbations on health-related quality of life at 1 year⁷
An exacerbation is the most important adverse event in the progression of COPD. It is a common cause of death, hospital admission, increased healthcare costs and decreased lung function. Consequently, it also has a negative impact on health-related quality of life (HRQoL). At least half of all COPD exacerbations, identified as symptom worsening, were not medically reported. More than one unreported exacerbation was already associated with a significantly (statistically and clinically) worse HRQoL. This suggests that unreported exacerbations, even though being associated with less symptom worsening than reported exacerbations, may have an important long-term impact of patients’ physical activities.
Elevated blood eosinophils in acute COPD exacerbations: better short-and long-term prognosis⁸
Elevated blood eosinophils in COPD is recognized as a potential risk factor for exacerbations. However, the prognostic role of these elevated blood eosinophils during exacerbations of COPD is unclear. Within this study, short-term and long-term outcomes have been investigated in patients with exacerbations of eosinophilic phenotype compared with patients with low blood eosinophils. COPD exacerbations in patients with high blood eosinophil have a better short-term prognosis without higher risk of subsequent exacerbation. These eosinophilic exacerbations also show a lower three-year mortality.
The role of nebulised budesonide in the treatment of exacerbations of COPD⁹
This study was done to evaluate the hypothesis that nebulised budesonide (NB) might be an alternative method to systemic corticosteroids (SC) in the treatment of COPD patients with exacerbations (ECOB). Patients hospitalized due to ECOB (n=159) were randomised into three groups: group 1 received standard bronchodilator treatment (SBDT), group 2 received SC (40 mg prednisolone) plus SBDT, and group 3 received NB (1,500 μg q.i.d.). During the upcoming 10-day hospitalization, improvements were compared with exacerbation and rehospitalisation rates after discharge. The study demonstrates that nebulised budesonide may be an effective and safe alternative to systemic corticosteroids in the treatment of exacerbations of chronic obstructive pulmonary disease.
The role of nebulized therapy in the management of COPD: evidence and recommendation¹⁰
In routine clinical practice, critical errors in using handheld inhalers are highly common and therefore frequently results in inadequate symptom relief. Current evidence concerning using nebulizer use for maintenance therapy in patients with moderate-to-severe COPD (including use during exacerbations), suggests that the efficacy of long-term nebulizer therapy is similar, and in some ways superior to that with pMDI/DPIs. Therefore, maintenance therapy with nebulizers may be well recommended for elderly patients, those with severe disease and frequent exacerbations, and those with physical and/or cognitive limitations.
Main takeaways
Chronic Obstructive Pulmonary Disease (COPD)
Global Initiative for Chronic Obstructive Lung Disease (GOLD) documents the global strategy for the Diagnosis, Management and Prevention of COPD. These guidelines are aimed at assisting healthcare professional in selecting the best strategy.²
300 million people worldwide are affected by COPD.³
Ambient air pollution increases the risk of respiratory mortality, is associated with lower lung function and increased COPD prevalence.⁴
COPD patients are often caught in a downward spiral, mainly due to exercise limitations.⁵
Exacerbations due to COPD generate a mean of 5.1 medical visits/year.⁶
Exacerbation is a common cause of death, hospital admission, increased healthcare costs and decreased lung function.⁷
At least half of all COPD exacerbations (identified as symptom worsening), were not medically reported.⁷
Elevated blood eosinophils in COPD are recognized as a potential risk factor for exacerbations.⁸
Maintenance therapy with nebulizers may be well recommended for elderly, those with severe diseases and frequent exacerbations, and those with physical and/or cognitive limitations.¹⁰
Comorbidities of Chronic Obstructive Pulmonary Disease
Common risk factors for COPD are age and smoking, which often lead to COPD patients to demonstrate multiple coexisting comorbidities.
Comorbidities in these patients are often responsible for impairing quality of life, increasing mortality in end-stage patients and increasing health costs. COPD comorbidities include diseases that independently coexist with COPD with no other causation, diseases that share common risk factors and pathogenetic pathways with COPD, diseases that are complicated by the interaction with the lung, and systemic manifestations of COPD. Therefore, no universal definition of COPD comorbidities has yet been accepted.¹¹
Obesity
COPD and obesity are both medical conditions that lead to slowly declining health. Due to the breathing difficulties that come with COPD, body’s oxygen supply can reduce which causes fatigue. Fatigue causes exercise intolerance and can therefore lead to a sedentary lifestyle, which further facilitates obesity.
Overweight in patients with chronic obstructive pulmonary disease needs more attention: a cross-sectional study in general practice.¹²
Although weight loss is common in patients with COPD, previous studies have shown that about 65% of the COPD population is overweight or obese. Overweight and obesity are highly prevalent in patients with milder stages of COPD. This cross-sectional study examines the association of overweight and obesity with the prevalence of comorbid disorders, in patients with mild to moderate COPD. They found, for example, that in all weight categories hypertension, osteoarthritis and diabetes are the highest prevalent comorbid disorders. Further examination of the results can be found in this article.
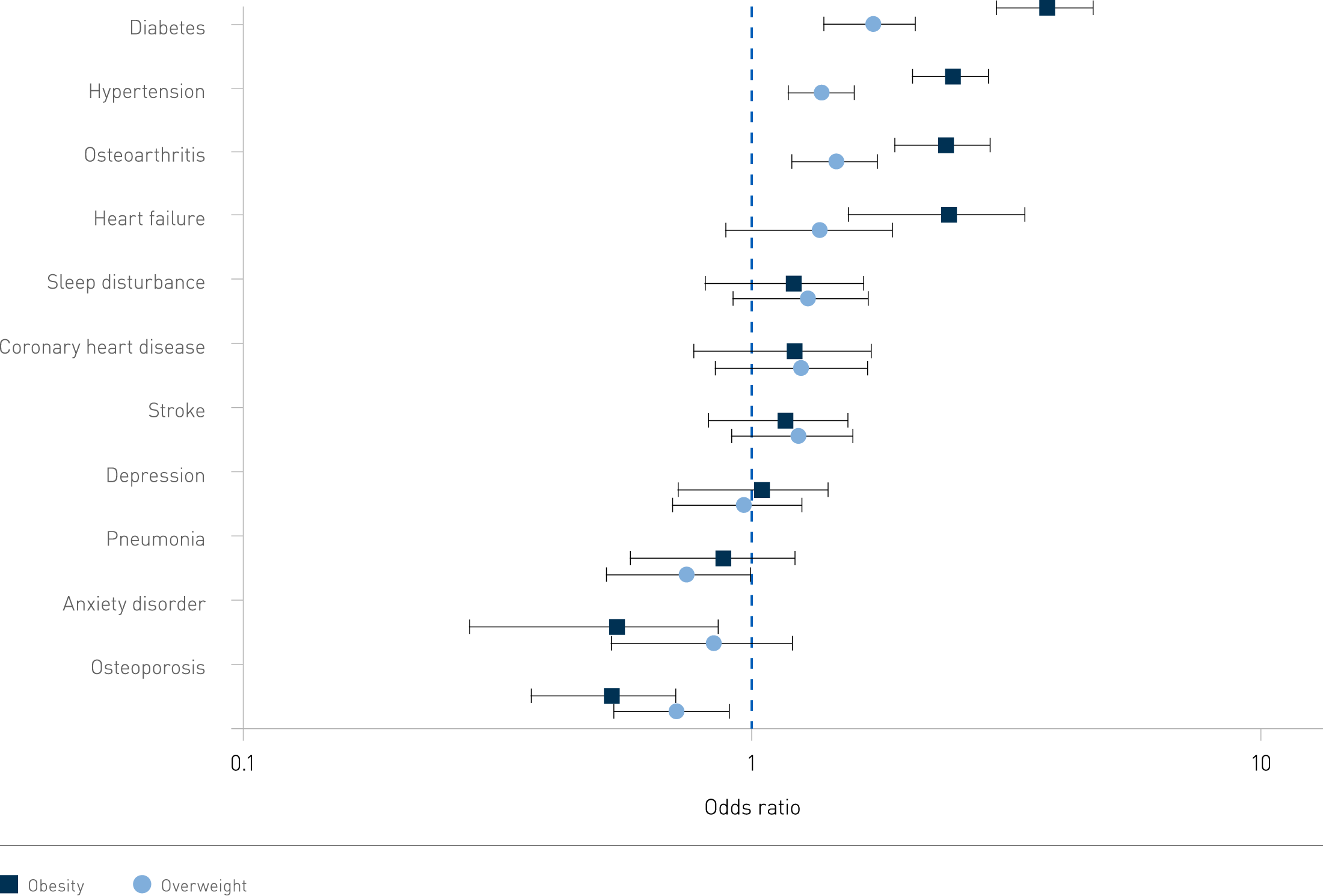
Adjusted odds ratios for the association of weight and comorbid disorders in patients with mild to moderate chronic obstructive pulmonary disease. The black dots represent the odds ratios (ORs) for the prevalence rate of comorbid disorders in overweight and obese patients, using the normal weight patients as reference category. The ORs are adjusted for clustering effect of general practice, gender, age, smoking status, and lung function. The error bars present the 95% confidence intervals around the ORs.
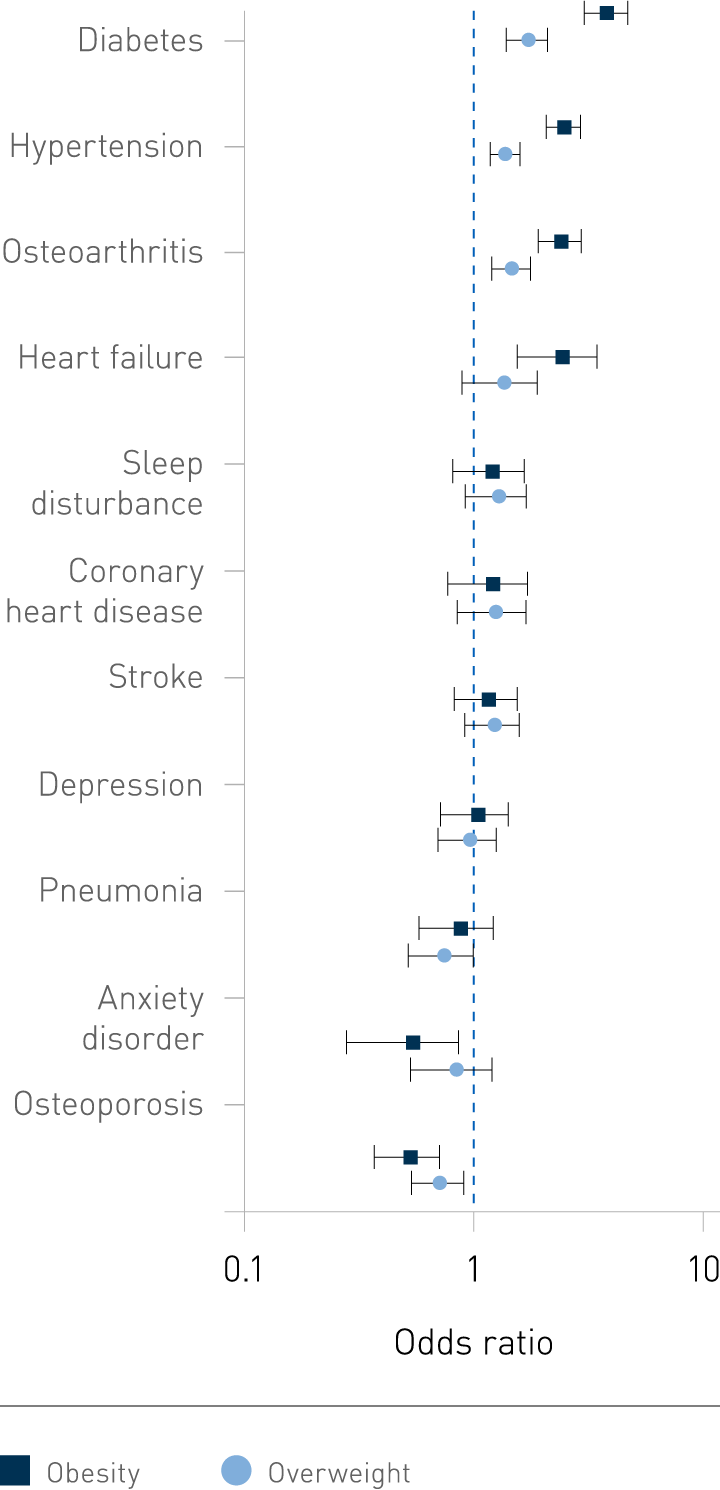
Adjusted odds ratios for the association of weight and comorbid disorders in patients with mild to moderate chronic obstructive pulmonary disease. The black dots represent the odds ratios (ORs) for the prevalence rate of comorbid disorders in overweight and obese patients, using the normal weight patients as reference category. The ORs are adjusted for clustering effect of general practice, gender, age, smoking status, and lung function. The error bars present the 95% confidence intervals around the ORs.
The impact of Obesity on Nighttime Blood Pressure Dipping¹³
Obesity not only increases arterial hypertension risk, but also has an impact on the response to antihypertensives. This study aimed to assess blood pressure parameters based on Ambulatory Blood Pressure Measurement in obese patients. They found that patients with extreme morbid obesity frequently exhibit hypertension of the reverse-dipping pattern. Reverse-dippers are characterized by the worst cardiovascular prognosis and outcomes, such as stroke and cardiovascular events. This study therefore highlights the importance of monitoring and managing nocturnal hypertension in obese patients, and thus also obese COPD-patients.
Heart Failure
Heart failure (HF) is a clinical syndrome which is caused by functional and structural defects in myocardium. These defects then result in impairment of ventricular filling or the ejection of blood. Most common cause of HF is reduced left ventricular myocardial function. However, dysfunction of the pericardium, myocardium, endocardium, heart valves or great vessels alone or combined is also associated with HF.¹⁴
The association between COPD and heart failure risk: a review¹⁵
COPD and heart failure frequently coexist in clinical practice. They share the same risk factors, which includes smoking, advanced age, and systemic inflammation. Among patients with HF, the prevalence of COPD ranges from 20 to 32%, and 10% of HF patients being hospitalized also suffer from COPD. On the other side, among COPD patients HF is prevalent in more than 20% of the patients. The risk ratio of developing HF among COPD patients is 4.5 times higher than those without the disease (after adjusting for age and other cardiovascular risk factors). Important to consider when looking at these numbers is that most studies use inappropriate definitions for COPD and HF. Nonetheless, identifying both diseases at an early stage is crucial. This article further reviews the physiopathology, clinical aspects, diagnosis, and treatment of patients with both conditions.
Pulmonary Hypertension
Pulmonary hypertension is a condition where blood pressure within the arteries of the lungs is increased. Symptoms that occur can vary from shortness of breath, chest pain, and light-headedness.
Detection of right sided heart changes and pulmonary hypertension in COPD patients¹⁶
Pulmonary hypertension is considered one of the common complications of COPD. Both are pathologically interdependent. COPD-associated pulmonary hypertension is a poor prognostic marker; it is associated with an increased risk of exacerbations, worsened exercise capacity, oxygenation, and mortality. The overall prevalence of pulmonary hypertension in COPD ranges from 20 to 63%. This present study was conducted on COPD patients to assess the function of the right side of the heart along with diagnosing pulmonary hypertension, studying hemodynamic abnormalities and functional limitations. Concluding that pulmonary hypertension in COPD patients is a co-morbidity with right sided changes. These patients had worse prognosis than COPD patients without pulmonary hypertension.
Osteoporosis
Osteoporosis is a condition that weakens bones, making them fragile and brittle, causing them to easily break. It is characterized by low bone mass and microarchitectural deterioration of bone tissue.
Osteoporosis in COPD: Are Bones Brittle in COPD?¹⁷
Osteoporosis becomes more prevalent in COPD patients as the disease progresses. The presence of various risk factors causes this, such as low body mass index, immobility due to decrease muscle mass, respiratory dysfunction, smoking and hypogonadism steroid either systemic or inhalational. A significant correlation between BMI and prevalence of osteoporosis was seen, lower body mass index had higher prevalence. Furthermore, an increase in severity of COPD also showed a statistically significant increase in percentage of osteoporosis at whole body level and at right femur.
Diabetes-type-2
Diabetes is a chronic condition that occurs when the pancreas does not produce enough insulin or when the body cannot effectively use the insulin it produces. The presence of comorbidity in older diabetes patients is common. Around half of the patients will have three or more comorbid chronic conditions.
Chronic obstructive pulmonary disease and diabetes mellitus: a systematic review of the literature.¹⁸
The relationship between type-2 diabetes mellitus (T2DM) and chronic obstructive pulmonary disease (COPD) remains complex. Recent studies have shown that T2DM can worsen the progression and prognosis of COPD, possibly due to the direct effects of hyperglycaemia on lung physiology, inflammation, or susceptibility to bacterial infection. Conversely, some evidence also show that COPD increases the risk of developing T2DM because of inflammatory processes and/or the therapeutic side effects which are related to the use of high-dose corticosteroids.
Anxiety and Depression
According to large population-based surveys, up to 33.7% of the population are affected by an anxiety disorder during their life. Depression currently affects more than 264 million people. About 85% of patients with depression have significant anxiety, and 90% of patients with anxiety disorder have depression. Depression and anxiety cause a high degree of emotional distress and functional impairment.¹⁹ ²⁰
Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructively pulmonary disease²¹
More than one third of individuals with COPD experience comorbid symptoms of depression and anxiety. Most common symptoms of depression include depressed mood and loss of interest and pleasure in daily activities. Anxiety is associated with physical and psychological discomfort, with symptoms such as fear, anxiety, and avoidance. Meta-analysis found that one in four COPD patients experience clinically significant depressive symptoms (compared with less than one in eight of the controls). Clinical anxiety in COPD patients has an estimated prevalence of up to 40%.
The Impact of Depression and Anxiety on Chronic Obstructive Pulmonary Disease Acute Exacerbations: A prospective cohort study.²²
This study explores the impact of anxiety and depression in COPD patients on the risk of acute exacerbation. An acute exacerbation is usually triggered by respiratory infection, air pollution and so on. An exacerbation results in a reduced health-related quality of life, pulmonary function and sustained worse health status. Within this study they discovered that there was a higher risk of acute exacerbation in COPD patients with anxiety (54.1%) compared to patients with no anxiety (39.8%). This is the same for patients with depression (52.1%) and patients without (40.4%). The COPD patients with anxiety and/or depression suffered higher risk of one acute exacerbation averagely during the one year.
Main takeaways
Comorbidities of Chronic Obstructive Pulmonary Disease
About 65% of the COPD population is overweight or obese.¹²
Patients with extreme morbid obesity frequently exhibit hypertension of the reverse-dipping pattern.¹³
COPD and heart failure frequently coexist, among COPD patients HF is prevalent in more than 20%.¹⁵
Pulmonary hypertension is considered one of the common complications of COPD.¹⁶
COPD-associated pulmonary hypertension is associated with increased risk of exacerbations, worsened exercise capacity, oxygenation, and mortality.¹⁶
An increase in severity of COPD also showed a statistically significant increase in percentage of osteoporosis at whole body level and at right femur.¹⁷
Studies have shown that COPD increases the risk of developing T2DM.¹⁸
More than one third of individuals with COPD experience comorbid symptoms of depression and anxiety.²¹
Patients with COPD and anxiety and/or depression suffered higher risk of one acute exacerbation averagely in one year.²²



