Clinical Research & Literature — Cardiology
Comorbidities of Cardiovascular Conditions
Comorbidity is a major public health issue, which challenges healthcare configured around single diseases.

Clinical Research & Literature — Cardiology
Comorbidities of Cardiovascular Conditions
Comorbidity is a major public health issue, which challenges healthcare configured around single diseases.
This study aims to provide an overview of frequent disease combinations of one and two additional chronic diseases and groups among patients with cardiovascular disease (CVD) in general practice. It concludes that comorbid conditions are very common in patients with CVD, even in younger age groups. To ensure efficient and effective treatment, organisational adaptations may be required in the healthcare system to accommodate comorbid conditions in patients with CVD.¹
Comorbidity
Comorbidity in patients with cardiovascular disease in primary care: a cohort study with routine healthcare data¹
Comorbidity is a major public health issue, which challenges healthcare configured around single diseases. This study aims to provide an overview of frequent disease combinations of one and two additional chronic diseases and groups among patients with cardiovascular disease (CVD) in general practice. It concludes that comorbid conditions are very common in patients with CVD, even in younger age groups. To ensure efficient and effective treatment, organisational adaptations may be required in the healthcare system to accommodate comorbid conditions in patients with CVD.
Resistant Hypertension
Resistant hypertension is defined as failure to achieve target blood pressure (BP) when a patient adheres to the maximum tolerated doses of three antihypertensive drugs including a diuretic.²
Resistant Hypertension an Overview of Evaluation and Treatment²
The prevalence of resistant hypertension is projected to increase, owing to the aging population, and increasing trends in obesity, sleep apnoea, and chronic kidney disease. Management of resistant hypertension must begin with a careful evaluation of the patient to confirm the diagnosis and exclude factors associated with “pseudo-resistance”, such as improper BP measurement technique, the white-coat effect, and poor patient adherence to lifestyle and/or antihypertensive medications. This paper provides an overview of evaluation and treatment of resistant hypertension.
Obstructive sleep apnoea
Obstructive sleep apnoea is a condition causing breathing to stop involuntarily for a brief period during sleep. It is a global issue with several implications on global health and quality of life.³
Epidemiological aspects of obstructive sleep apnoea³
At an individual level, obstructive sleep apnoea (OSA) leads to a significant decrease in quality of life (QOL) and functional capacity, alongside a markedly increased risk of cardiovascular disease and death. At a societal level, OSA not only leads to reduced economic productivity, but also constitutes a major treatable risk factor for hypertension, coronary artery disease (CAD) and stroke. This article addresses OSA from an epidemiological perspective, from prevalence studies to economic aspects to co-morbidity.
Treatment options for obstructive sleep apnoea⁴
Obstructive sleep apnoea (OSA) is a global problem with implications for general health and of life, and is often encountered in patients with neurologic disease. This review outlines treatment modalities to consider for management of OSA in patients with neurologic disease. New advances in positive airway pressure (PAP) devices, oral appliances, and surgical interventions offer a wide range of treatment options for patients with OSA.
Obstructive sleep apnoea and Obesity: Implications for Public Health⁵
Obstructive sleep apnoea (OSA) is a global disease with a rising incidence along with its comorbidities, especially with metabolic syndrome. One of the main components contributing to sleep apnoea is obesity, as well as diabetes mellitus type 2 (T2DM), hypercholesterolemia, and hypertension. This paper addresses important public health implications to prevent and to treat the condition.
Association Between Treated and Untreated Obstructive Sleep Apnoea and Risk of Hypertension⁶
Systemic hypertension is prevalent among patients with obstructive sleep apnoea (OSA). Short-term studies indicate that continuous positive airway pressure (CPAP) therapy reduces blood pressure in patients with hypertension and OSA. The objective of the study is to determine whether CPAP therapy is associated with lower risk of incident hypertension. It concludes that compared to people without OSA the presence of OSA was associated with increased adjusted risk of incident hypertension; however, treatment with CPAP therapy was associated with a lower risk of hypertension.
Obstructive sleep apnoea and its cardiovascular consequences⁷
Obstructive sleep apnoea (OSA) is a common disorder in which repetitive apnoea’s expose the cardiovascular system to cycles of hypoxia, exaggerated negative intrathoracic pressure, and arousals. Epidemiological studies have shown significant independent associations between OSA and hypertension, coronary artery disease, arrhythmias, heart failure, and stroke. This article will review our current understanding of mechanisms by which OSA might contribute to the pathogenesis of cardiovascular disease, it will assess epidemiological evidence concerning a potential link between these two conditions and it reviews cardiovascular effects of treating OSA.
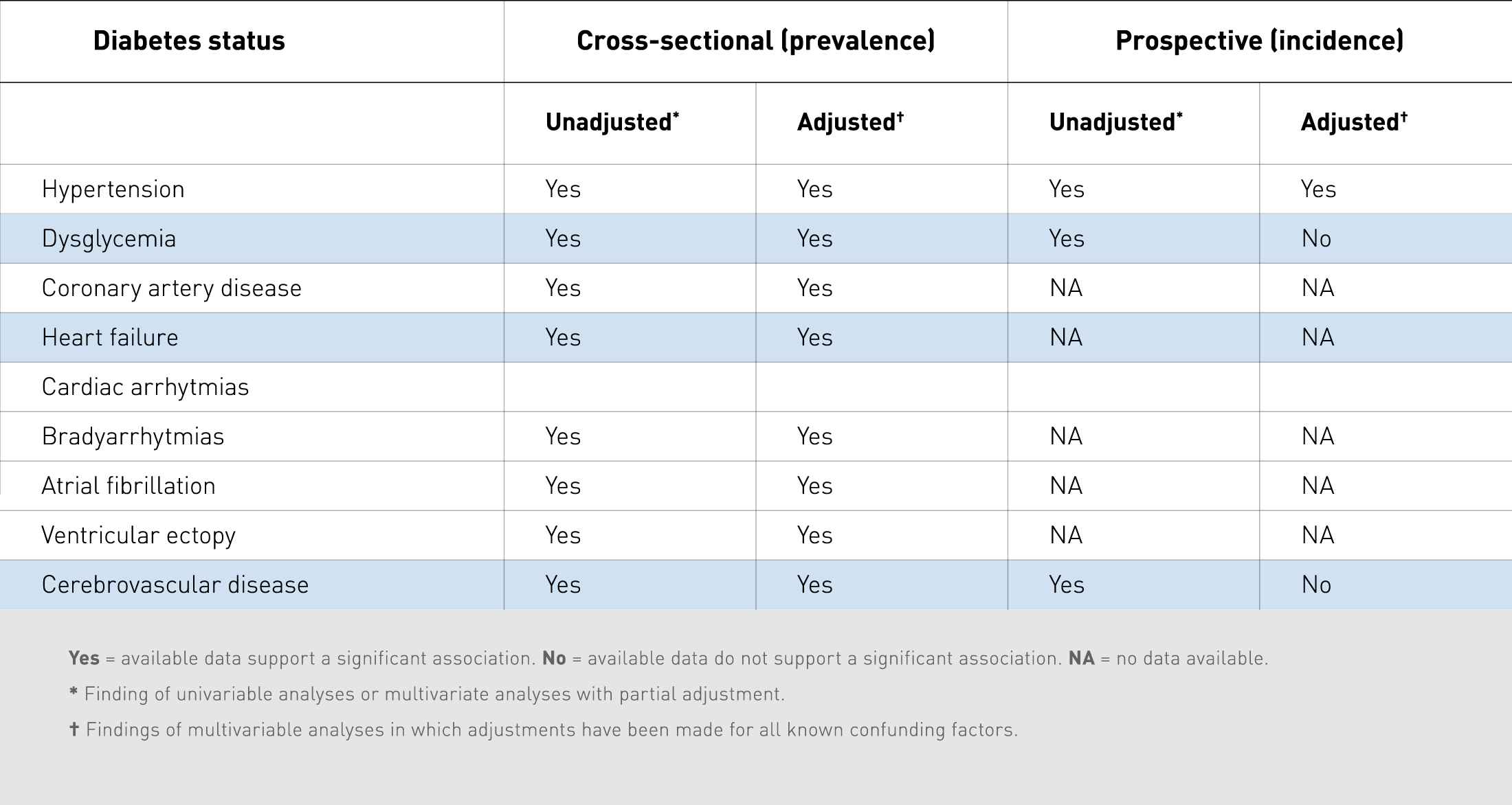
Summary of community-based epidemiological studies investigating the potential links between obstructive sleep apnoea and cardiovascular diseases⁷
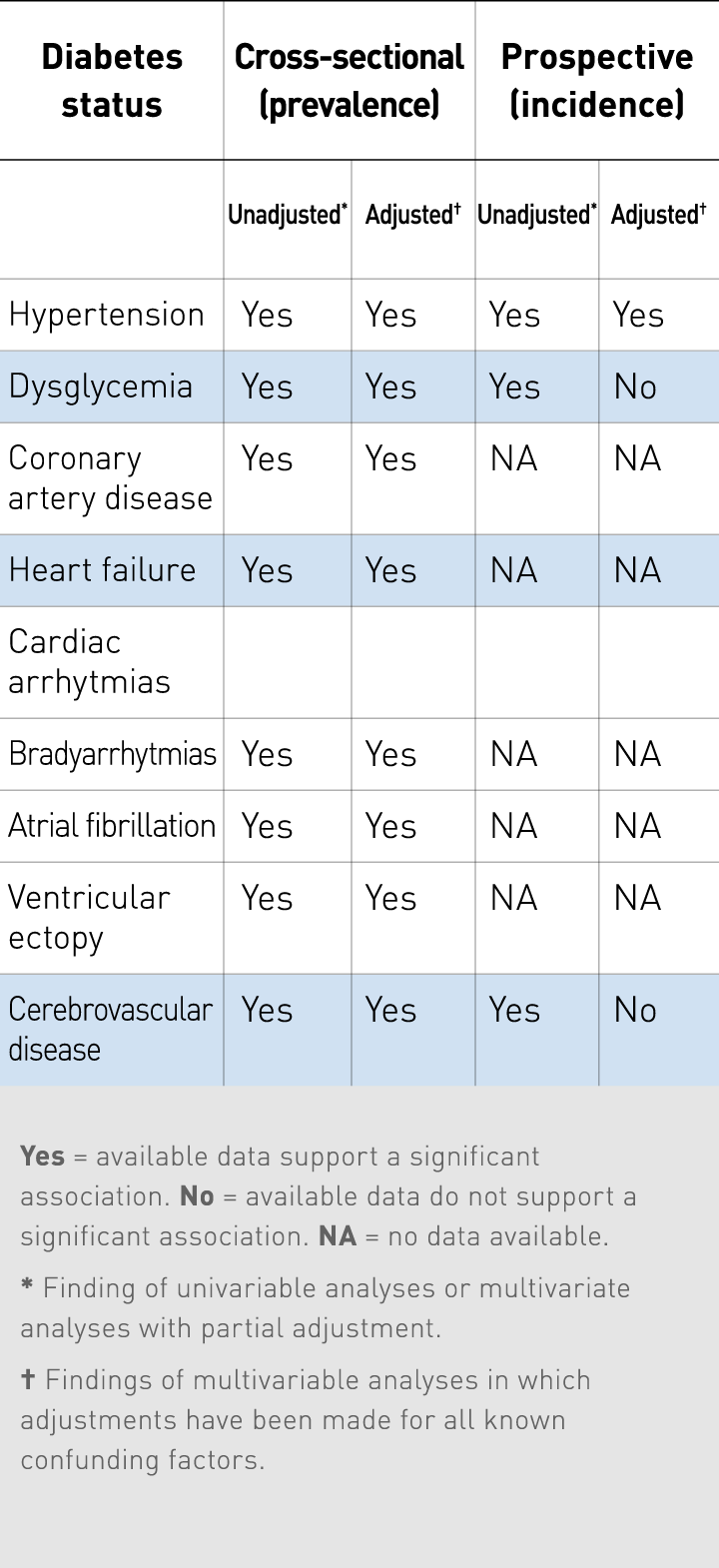
Summary of community-based epidemiological studies investigating the potential links between obstructive sleep apnoea and cardiovascular diseases⁷
Main takeaways
Obstructive sleep apnoea
Obstructive sleep apnoea (OSA) is characterized by recurrent episodes of upper airway obstruction occurring during sleep.³
Obstructive sleep apnoea leads to significant decrease in quality of life and functional capacity, alongside a markedly increased risk of cardiovascular disease and death.⁵
Due to the increasing prevalence of obesity globally, the number of people with OSA will also increase. There is a linear correlation between OSA and obesity.⁵
Patients with OSA are more likely to develop hypertension and the risk is associated with the severity of OSA.⁶
Data from animal models, epidemiological studies, and randomised clinical trials provide strong evidence that OSA can cause hypertension, and that its treatment can lower blood pressure.³
Chronic kidney disease
Chronic kidney disease (CKD) is an important and common noncommunicable condition globally. It refers to a long-term loss of renal function and is categorised in stages.
Global Prevalence of Chronic Kidney Disease – A Systematic Review and Meta-Analysis⁸
Chronic kidney disease (CKD) is a global health burden with a high economic cost to health systems and is an independent risk factor for cardiovascular disease (CVD). All stages of CKD are associated with increased risks of cardiovascular morbidity, premature mortality, and/or decreased quality of life. CKD is usually asymptomatic until later stages, and accurate prevalence data are lacking. This systematic review and meta-analysis of observational studies estimating CKD prevalence in general populations was conducted through literature searches in 8 databases.
Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: meta-analysis of randomised controlled trials⁹
Chronic kidney disease, most defined by a reduced glomerular filtration rate (GFR) or abnormal concentrations of proteinuria, or both, is an important public health problem, affecting 10-15% of the adult general population. The objective of this article is to define the cardiovascular effects of lowering blood pressure in people with chronic kidney disease. It concluded that blood pressure lowering is an effective strategy for preventing cardiovascular events among people with moderately reduced eGFR.
Chronic kidney disease: identification and management in primary care¹⁰
We distinguish between five stages of chronic kidney disease. With treatment and lifestyle changes, the progression through the stages can be slowed down and the patient can also prevent their condition from worsening. It is often asymptomatic in its early stages, and early detection is important to reduce future risk. The risk of cardiovascular outcomes is greater than the risk of progression to end-stage kidney disease for most people with CKD. This review aims to summarize the vital role that primary care plays in pre-dialysis CKD care and to outline the main considerations in its identification, monitoring, and clinical management in this context.
Nocturnal Systolic Hypertension and Adverse Prognosis in Patients with CKD¹¹
Nocturnal hypertension is associated with adverse outcomes in patients with CKD. However, the individual association of entities of nocturnal hypertension according to achievement of systolic and/or diastolic BP goals with kidney failure and cardiovascular outcomes of CKD is not clear. The purpose of this study was to evaluate the individual prognostic value of nocturnal hypertension entity in a large, prospective cohort of Chinese patients with CKD not on dialysis. It concludes that nocturnal systolic hypertension, either alone or in combination with diastolic hypertension, is associated with higher risks for adverse outcomes in patients with CKD.
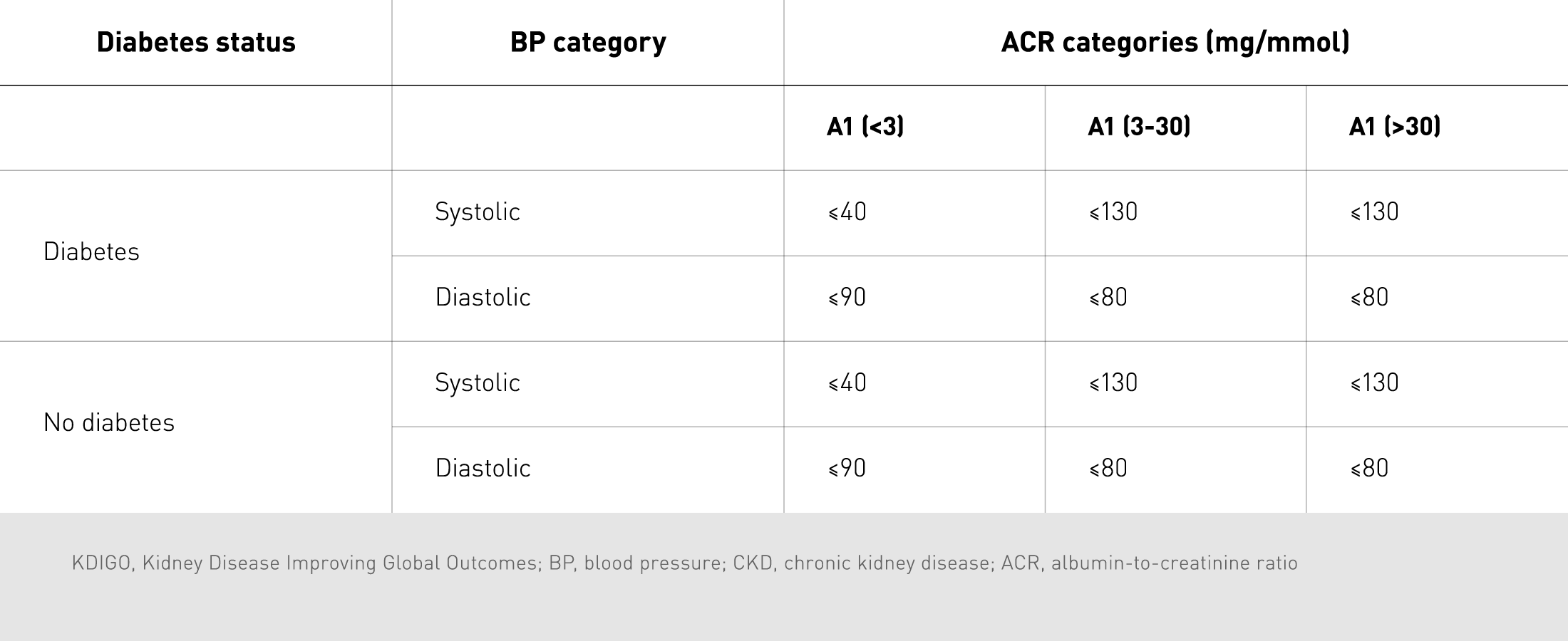
KDIGO recommended BP targets for people with CKD¹⁰
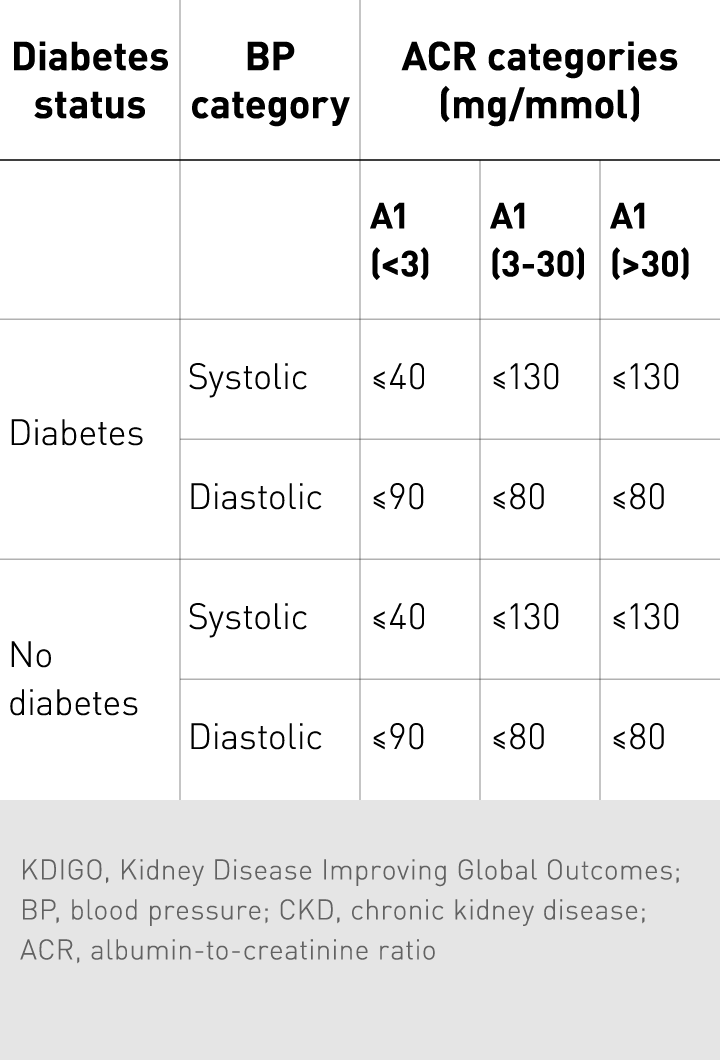
KDIGO recommended BP targets for people with CKD¹⁰
Main takeaways
Chronic kidney disease
All stages of CKD are associated with increased risks of cardiovascular morbidity, premature mortality, and/or decreased quality of life.⁸
Blood pressure lowering is an effective strategy for preventing cardiovascular events among people with moderately reduced eGFR.⁹
CKD patients mostly have a comorbidity such as hypertension, diabetes, and heart failure.⁸
Primary care plays a crucial role in pre-dialysis CKD care and in outlining the main considerations in its identification, monitoring, and clinical management.¹⁰
Nocturnal systolic hypertension, either alone or in combination with diastolic hyper-tension, is associated with higher risks for adverse outcomes in patients with CKD.¹¹
Metabolic syndrome
Metabolic Syndrome is a constellation of anthropometric, haemodynamic, and metabolic abnormalities.
The Metabolic Syndrome and Cardiovascular Risk:
A Systematic Review and Meta-Analysis¹²
The objective of this study is to conduct a systematic review and meta-analysis of the cardiovascular risk associated with the metabolic syndrome as defined by the 2001 National Cholesterol Education Program (NCEP) and 2004 revised National Cholesterol Education Program (rNCEP). It concludes that metabolic syndrome is associated with a 2-fold increase in cardiovascular outcomes and a 1.5-fold increase in all-cause mortality.
The metabolic syndrome, its component risk factors, and progression of coronary atherosclerosis¹³
Although there is accelerated disease progression observed in patients with metabolic syndrome, according to this study, it appears to be largely driven by individual component risk factors rather than by the presence of metabolic syndrome itself. This provides further support for the concept that conferring a diagnosis of metabolic syndrome highlights a patient with multiple atherogenic risk factors.
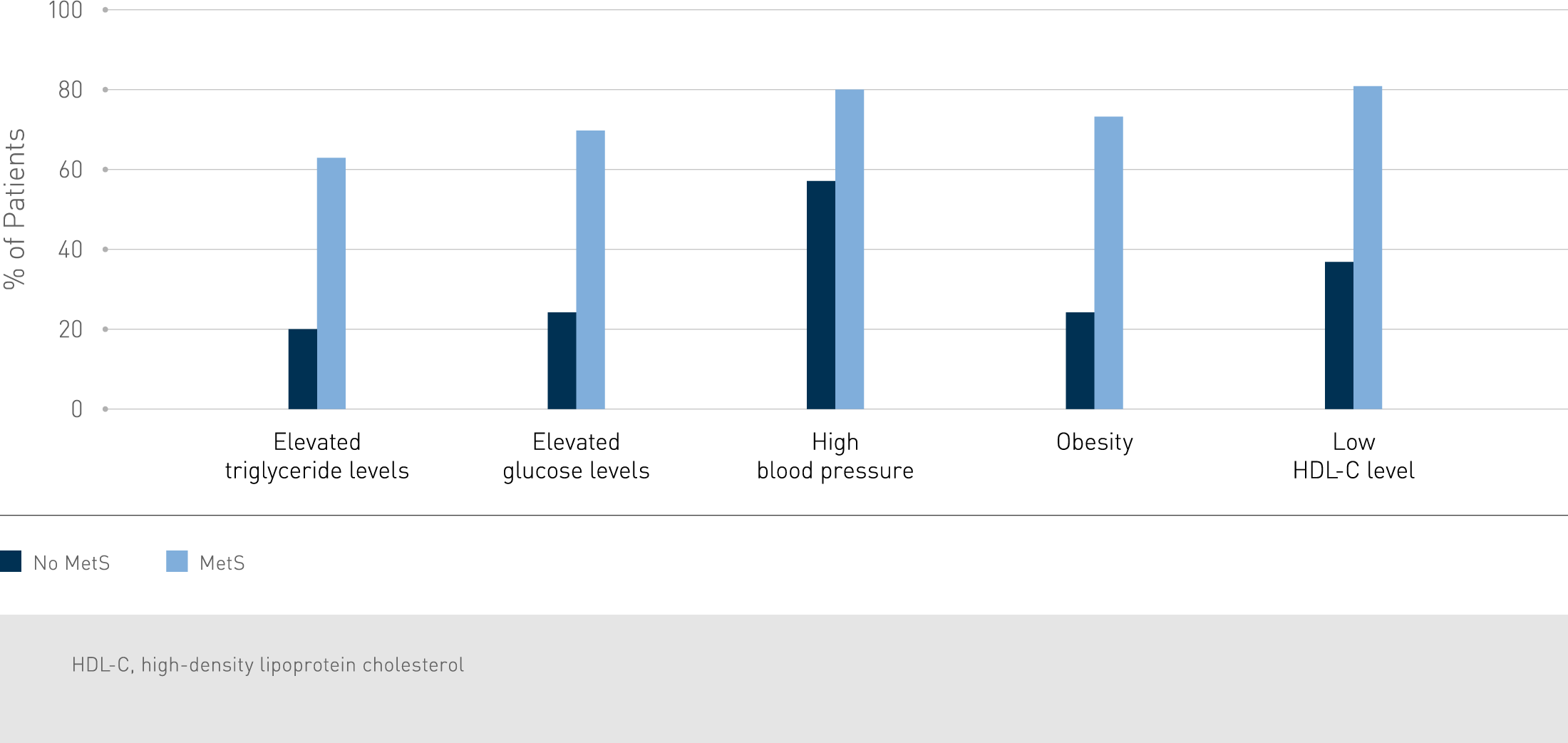
Percentage of patients with or without metabolic syndrome (MetS) with each defining component risk factor.1 HDL-C, high-density lipoprotein cholesterol
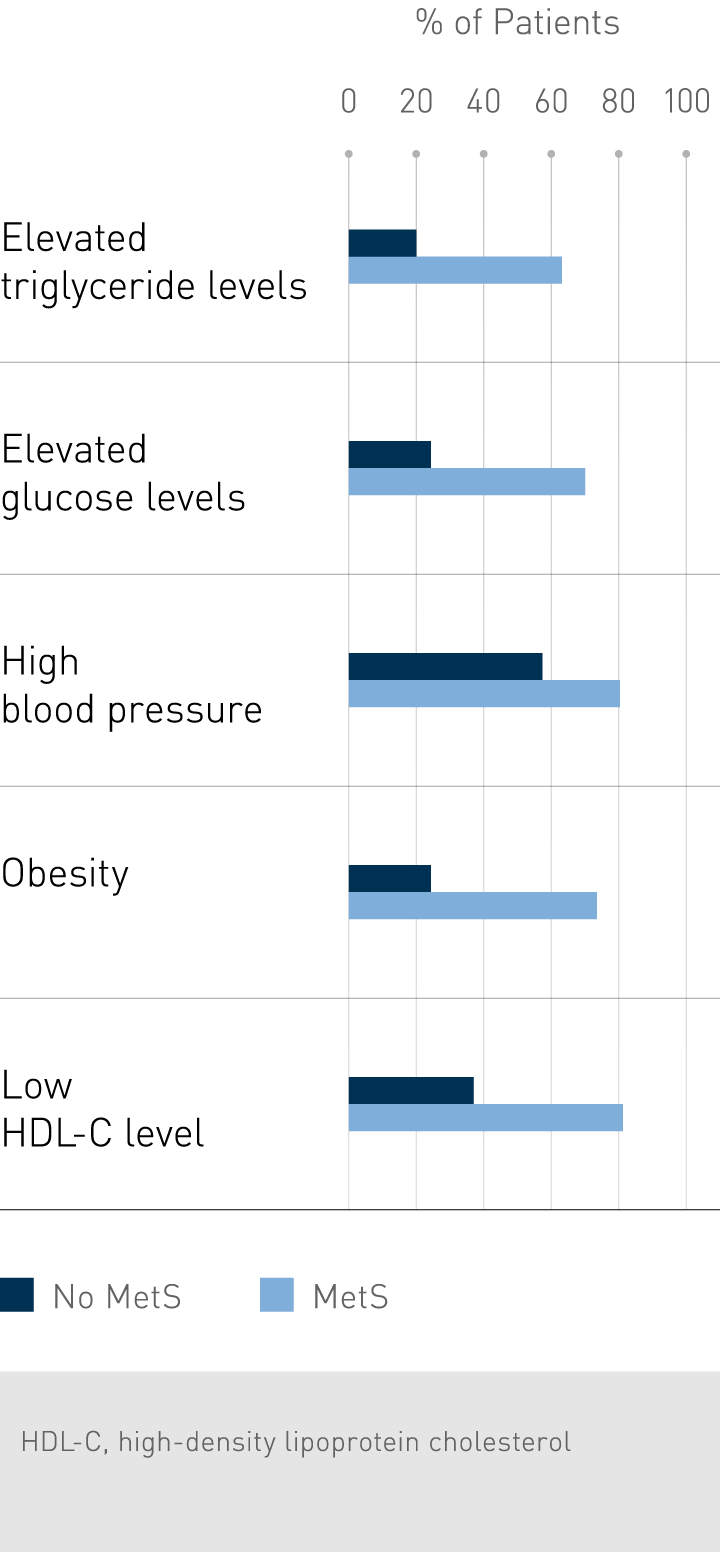
Percentage of patients with or without metabolic syndrome (MetS) with each defining component risk factor.1 HDL-C, high-density lipoprotein cholesterol
Treatment of metabolic syndrome¹⁴
This review focuses on the treatment of the metabolic syndrome. Diagnosing patients with metabolic syndrome allows them to make the necessary lifestyle changes, such as losing weight and reducing abdominal obesity. This is the main therapeutic goal in metabolic syndrome. Even though intensive lifestyle changes will help in normalizing a patient’s lipid profile, some patients might need drug therapy if this is not sufficient. It is recommended to prescribe anti-hypertensive drugs in [mild] hypertensive patients with metabolic disturbances when systolic blood pressure is ≥ 140 and/or diastolic blood pressure is ≥90 mmHg after a suitable period of lifestyle change.
Main takeaways
Metabolic syndrome
Metabolic syndrome is associated with a 2-fold increase in cardiovascular outcomes and a 1.5-fold increase in all-cause mortality.¹²
Metabolic syndrome appears to be largely driven by individual component risk factors rather than by the presence of metabolic syndrome itself.¹³
The main therapeutic goal for metabolic syndrome is lifestyle changes such as losing weight and reducing abdominal obesity. However, some patients still might need drug therapy.¹⁴
Diabetes
Diabetes mellitus is defined as a group of metabolic diseases characterized by chronic hyperglycaemia because of defects in insulin secretion, insulin action, or both. Hypertension and diabetes often coexist and the risk of developing cardiovascular diseases is four-fold higher with both conditions. The prevalence of diabetes is increasing worldwide.
Diabetes mellitus: The epidemic of the century¹⁵
In this article, the epidemic nature of diabetes mellitus in different regions is reviewed. Diabetes mellitus is rising to an alarming epidemic level. Early diagnosis of diabetes and prediabetes is essential using recommended haemoglobin A1c criteria for different types except for gestational diabetes. Screening for diabetes especially in underdeveloped countries is essential to reduce late diagnosis.
Diabetes and Hypertension: Is There a Common Metabolic Pathway?¹⁶
Diabetes and hypertension frequently occur together. There is substantial overlap between diabetes and hypertension in etiology and disease mechanisms. Obesity, inflammation, oxidative stress, and insulin resistance are thought to be the common pathways. Recent advances in the understanding of these pathways have provided new insights and perspectives. Physical activity plays an important protective role in the two diseases. Knowing the common causes and disease mechanisms allows a more effective and proactive approach in their prevention and treatment.
Type 2 diabetes mellitus and hypertension: An update¹⁷
Diabetes is common in hypertensive patients and an increased prevalence of hypertension was noted in diabetic patients. Both conditions exacerbate one another, due to which it is important to understand their co-occurrence and the best treatments recommended to control it. The risk for cardiovascular disease (CVD) is four-fold higher in patients with both diabetes and hypertension as compared to the normotensive non-diabetic controls.
Blood Pressure Lowering in Type 2 Diabetes – A Systematic Review and Meta-analysis¹⁸
Lowering blood pressure (BP) is widely used to reduce vascular risk in individuals with diabetes. The objective of this study is to determine the associations between BP–lowering treatment and vascular disease in type 2 diabetes. Supporting the use of BP lowering medication, this review concludes that among patients with type 2 diabetes, BP lowering was associated with improved mortality rates and other clinical outcomes.
Main takeaways
Diabetes
Hypertension is common and dangerous in patients with diabetes.¹
The risk for cardiovascular disease (CVD) is four-fold higher in patients with both diabetes and hypertension as compared to the normotensive non-diabetic controls.¹⁷
Drug choices are marginally different from those used in essential hypertension.¹⁸
Treatment targets are a little uncertain but BP<140/90 mmHg would be a good starting point.¹⁸
Obesity
Worldwide least 400 million adults are obese and more than 20 million children under the age of 5 are overweight and the numbers are increasing. Obesity can lead to life-threatening issues, including hypertension, and treatment can be quite challenging.¹⁹
Obesity and hypertension (Review)¹⁹
The imbalance between energy intake and expenditure is the main cause of excessive overweight and obesity. Technically, obesity is defined as the abnormal accumulation of ≥20% of body fat, over the individual's ideal body weight. Excessive overweight remains among the most neglected public health issues worldwide, while obesity is associated with increasing risks of disability, illness and death. Cardiovascular diseases, the leading cause of mortality worldwide, particularly hypertension and diabetes, are the main illnesses associated with obesity. In this review, the researchers address the association between obesity and cardiovascular disease, particularly the biological mechanisms linking obesity and hypertension.
Influence of Weight Reduction on Blood Pressure – A Meta-Analysis of Randomized Controlled Trials²⁰
Increased body weight is a strong risk factor for hypertension. In this review a meta-analysis of randomized controlled trials was performed to estimate the effect of weight reduction on blood pressure overall and in population subgroups. This meta-analysis shows that weight loss is important for the prevention and treatment of hypertension.
The Kidney, Hypertension, and Obesity²¹
This paper brings forth a perspective of the role of abnormal renal pressure natriuresis in the pathogenesis of hypertension. Obesity increases renal sodium reabsorption and impairs pressure natriuresis by activation of the renin-angiotensin and sympathetic nervous systems and by altered intrarenal physical forces. Chronic obesity also causes marked structural changes in the kidneys that eventually lead to a loss of nephron function. It further increases arterial pressure and severe renal injury in some cases.
Which cuff should I use? Indirect blood pressure measurement for the diagnosis of hypertension in patients with obesity: a diagnostic accuracy review²²
This paper determines the diagnostic accuracy of different methods of blood pressure (BP) measurement compared with reference standards for the diagnosis of hypertension in patients with obesity with a large arm circumference. It concludes that BP measurement with a correctly fitting upper arm cuff is sufficiently sensitive and specific to diagnose hypertension in patients with obesity with a large upper arm circumference. If a correctly fitting upper arm cuff cannot be applied, an incorrectly fitting standard size cuff should not be used and BP measurement at the wrist should be considered.
Obesity Paradox in Patients with Hypertension and Coronary Artery Disease²³
An obesity paradox, a “paradoxical” decrease in morbidity and mortality with increasing body mass index (BMI), has been shown in patients with heart failure and those undergoing percutaneous coronary intervention. This paper shows that in a population with hypertension and coronary artery disease, overweight and obese patients had a decreased risk of primary outcome compared with patients of normal weight, which was driven primarily by a decreased risk of all-cause mortality. The results further suggest a protective effect of obesity in patients with known cardiovascular disease in concordance with data in patients with heart failure and those undergoing percutaneous coronary intervention.
Main takeaways
Obesity
The relationship between BMI and systolic and diastolic blood pressure is nearly linear.¹⁹
Weight loss is important for the prevention and treatment of hypertension.²⁰
The increase of renal tubular sodium reabsorption impairs pressure natriuresis and has an important role in initiating obesity hypertension.²¹
Obesity is associated with obstructive sleep apnoea and masked and white-coat hypertension.¹⁹
BP monitoring in obese patients requires a correctly fitting upper arm cuff, if this cannot be applied a BP measurement at the wrist should be considered.²²
The obesity paradox indicates that patients with hypertension, coronary artery disease and obesity showed fewer fatalities, non-fatal myocardial infarction and non-fatal stroke.²³



