Clinical Research & Literature — Cardiology
Blood Pressure Monitoring
Blood pressure monitoring can help with diagnosing and treating this condition.

Clinical Research & Literature — Cardiology
Blood Pressure Monitoring
Blood pressure monitoring can help with diagnosing and treating this condition.
High blood pressure comes with high risks. However, it often goes undetected until it’s too late. Blood pressure monitoring can help with diagnosing and treating this condition. Blood pressure is measured in units of millimetres of mercury (mmHg). The readings are always given in pairs, with the upper (systolic) value first, followed by the lower (diastolic) value. Different methods of blood pressure monitoring include clinical blood pressure monitoring, ambulatory blood pressure monitoring, and self-monitoring.¹
Office blood pressure monitoring
Auscultatory or oscillometer semiautomatic or automatic sphygmomanometers are the preferred method for measuring BP in the doctor’s office. With inadequate attention to the standardized conditions recommended for the valid measurement of office BP, it can be performed improperly. Improper measurement of office BP can lead to inaccurate classification, overestimation of a patient’s true BP, and unnecessary treatment.²
Masked Hypertension³
The addition of ambulatory blood pressure monitoring to conventional clinic measurement for defining blood pressure status in clinical practice has added a new complexity to the process. The separation of normotension and hypertension can be assessed independently by each of the two methods. We thus have four potential groups of patients who are, first, normotensive by both methods (true normotensives); second, hypertensive by both (true, or sustained, hypertensives); third, hypertensive by clinic measurement and normotensive by ambulatory measurement (white-coat hypertensives); and fourth, normotensive by clinic measurement and hypertensive by ambulatory measurement (masked hypertension). In this paper the importance of this fourth group will be addressed.
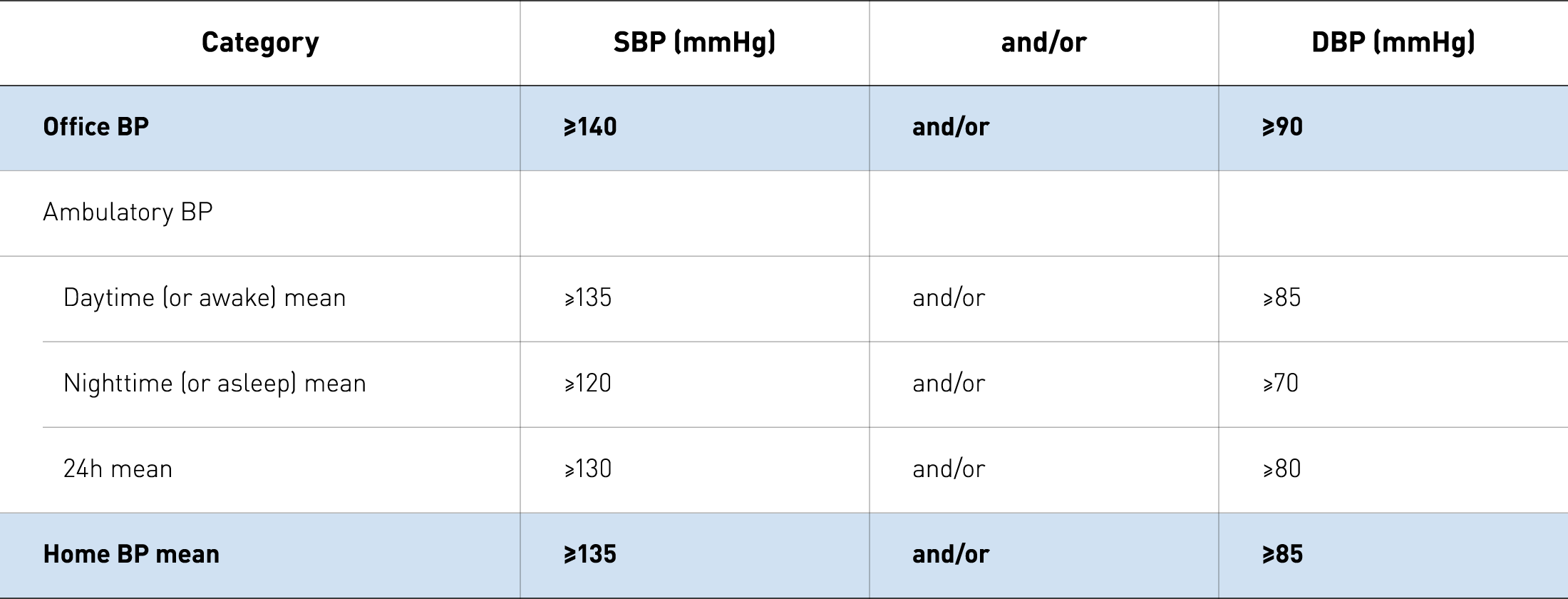
Definitions of hypertension according to office, ambulatory, and home blood pressure levels Category²
Definitions of hypertension according to office, ambulatory, and home blood pressure levels Category²
Masked hypertension: a systematic review⁴
The purpose of this research was to review the literature on masked hypertension. The prevalence of masked hypertension seems to lie between 8 and 20% and can be up to 50% in treated hypertensive patients. Subjects with masked hypertension have a higher risk of cardiovascular events than normotensive subjects. This is due to a possible failure to recognize and appropriately manage this form of hypertension, the frequent association with other risk factors and coexisting target organ damage.
White-Coat Hypertension – New Insights from Recent Studies⁵
White-coat hypertension indicates individuals who are not on treatment for hypertension but who had elevated office blood pressure and normal daytime blood pressure measured with ambulatory blood pressure monitoring (ABPM). Clearly, these individuals would be at low cardiovascular risk. The purpose of this review is to provide new insights into the characteristics, definitions, and cardiovascular risk assessment in persons with white-coat hypertension, and it will be limited primarily to ABPM with a primary focus on prospective studies.
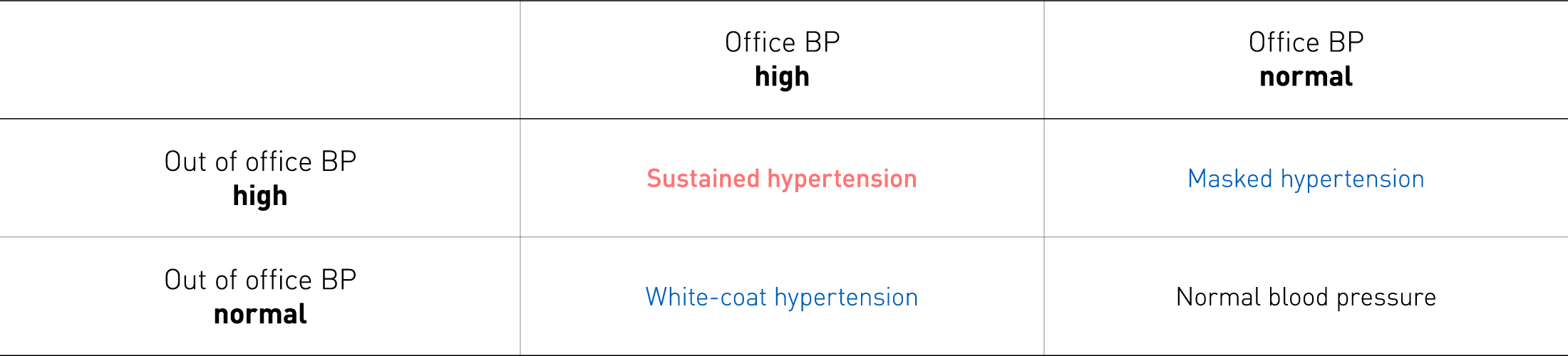
What is missed at the doctor’s office?²
What is missed at the doctor’s office?²
Ambulatory blood pressure monitoring
The ambulatory blood pressure is ideally measured every 15-30 minutes. Ambulatory monitoring is usually carried out over a 24-hour period. Day and night, awake and asleep, are either defined as clock times or by the time individuals say they sleep. Ambulatory blood pressure monitoring is still the golden standard for diagnosing hypertension and predicting hypertension-mediated organ damage. However, it is becoming less popular with patients to carry a device around for 24 hours. ABPM leads to decreased sleep quality during the night which can cause misleading readings. 24-hour measurement has been consistently shown to have a closer relationship with morbid or fatal events.² ¹³
European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring (ABPM)⁶
The article represents an updated schematic summary of the most important aspects related to the use of ABPM in daily practice, and is aimed at providing recommendations for proper use of this technique in a clinical setting by both specialists and practicing physicians. The clinical indications for ABPM suggested by the available studies, among with white-coat phenomena, masked hypertension, and nocturnal hypertension are outlined in detail. Furthermore, the place of home measurement of blood pressure in relation to ABPM is discussed.
Ambulatory blood pressure monitoring⁷
Any clinical measurement of blood pressure may be regarded as a surrogate measure for the “true” blood pressure of the patient, which may be defined as the mean level over prolonged periods. Two techniques have been developed to improve the estimate of true blood pressure — ambulatory monitoring and home monitoring (or self-monitoring). This article will focus on the implications of ambulatory monitoring.
Self-monitoring and Remote management
Self-monitoring or home blood pressure monitoring can provide a larger number of blood pressure measurements than conventional office measurements in conditions that are more representative of daily life. Available studies have further indicated that home measurements better predict cardiovascular morbidity and mortality than office blood pressure measurements.²
Call to Action on Use and Reimbursement for Home Blood Pressure Monitoring⁸
Home blood pressure monitoring (HBPM) overcomes many of the limitations of traditional office blood pressure (BP) measurement and is both cheaper and easier to perform than ambulatory BP monitoring. This call-to-action article makes several recommendations, including: HBPM should become a routine component of BP measurement in the majority of patients with known or suspected hypertension; Two to three readings should be taken while the subject is resting in the seated position, both in the morning and at night, over a period of one week. Read more about these interesting insights.
Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial⁹
This trial aimed to test a digital intervention for hypertension management in primary care by combining self-monitoring of blood pressure with guided self-management. The primary outcome was the difference in systolic blood pressure after one year. The study concludes that using self-monitored blood pressure led to better control of systolic blood pressure after one year than usual care, with low incremental costs.
Impact of Changes to National Hypertension Guidelines on Hypertension Management and Outcomes in the United Kingdom¹⁰
In recent years, national and international guidelines have recommended the use of out-of-office blood pressure monitoring for diagnosing hypertension. Despite evidence of cost-effectiveness, critics expressed concerns this would increase cardiovascular morbidity. This article is assessing the impact of these changes on the incidence of hypertension, out-of-office monitoring and cardiovascular morbidity. They used routine clinical data from UK general practices, linked to inpatient hospital, mortality and socio-economic status data. The changes to hypertension guidelines in 2011 were associated with a stabilisation in incidence and no increase in cardiovascular events. Guidelines should continue to recommend out-of-office monitoring for diagnosis of hypertension.
Effect of Self-monitoring and Medication Self-titration on Systolic Blood Pressure
in Hypertensive Patients at High Risk of Cardiovascular Disease: The TASMIN-SR Randomized Clinical Trial¹¹
This study establishes the effect of self-monitoring with self-titration of antihypertensive medication compared with usual care on systolic blood pressure among patients with cardiovascular disease, diabetes, or chronic kidney disease. The study concluded that indeed among patients with hypertension at high risk of cardiovascular disease, self-monitoring with self-titration of antihypertensive medication compared with usual care resulted in lower systolic blood pressure at 12 months.
Performance and persistence of a blood pressure self-management intervention: telemonitoring and self-management in hypertension (TASMINH2) trial¹²
This study aimed to evaluate, in detail, the implementation of the self-management intervention used in the TASMINH2 trial. The intervention, comprising self-monitoring for the first week of each month and an individualised treatment self-titration schedule, was developed from a previous trial of self-management. Although adherence to the intervention reduced over time, implementation of treatment recommendations appeared better than equivalent trials using physician titration. Future self-management interventions should aim to better support patients’ decision making, perhaps through enhanced use of technology.
Cost-Effectiveness of Telemonitoring and Self-Monitoring of Blood Pressure for Antihypertensive Titration in Primary Care (TASMINH4)¹³
The use of self-monitoring of blood pressure (with or without telemonitoring) has been recently demonstrated to reduce blood pressure compared to using clinic monitoring (current practice). This study assessed the cost-effectiveness of physician titration of antihypertensive medication using self-monitored blood pressure, with or without telemonitoring, to make hypertension treatment decisions in primary care compared with usual care. A Markov patient-level simulation model was developed taking a UK Health Service/Personal Social Services perspective. Concluding that self-monitoring in clinical practice is cost-effective and likely to lead to reduced cardiovascular mortality and morbidity.
OMRON’s Hypertension Plus
Supports clinicians to manage hypertensive populations more effectively.
Hypertension Plus includes unique clinical decision support tools based on NICE Guidelines and know-how from the TASMINH clinical trials. Guiding clinicians on when to act, and to provide a remote patient monitoring solution.


Blood pressure monitoring during pregnancy
Physiological changes during pregnancy lead to difficulties in obtaining accurate blood pressure readings. An understanding of these changes helps to diagnose and treat hypertensive disorders such as gestational, white-coat and masked hypertension, or pre-eclampsia.¹⁴
Hypertensive Disorders of Pregnancy – ISSHP Classification, Diagnosis, and Management Recommendations for International Practice¹⁵
Worldwide there is disagreement about many aspects of the classification, diagnosis,
and management of the hypertensive disorders of pregnancy. This set of recommendations provides practical advice on classification, diagnostic criteria, and management for all clinicians, who are involved in the management of women with hypertension during pregnancy.
The classification, diagnosis, and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP¹⁶
In the years since the ISSHP report mentioned above, there have been several developments relevant to diagnosis, classification, and management of the hypertensive disorders in pregnancy. One problem is the emerging concept that pre-eclampsia may indeed have several subtypes, the final clinical manifestation being the result of a maternal constitutive response to either abnormal placental function or abnormal placentation. This purpose of this article is to update the ISSHP on these new developments.
The natural history of white-coat hypertension during pregnancy¹⁷
White-coat hypertension (WCH) is a common phenomenon with a long-term prognosis intermediate between those with true hypertension and true normotension. The natural history of this phenomenon throughout pregnancy remains unknown. This article assessed the likelihood of women with an initial diagnosis of WCH developing pre-eclampsia (PE) as their pregnancy progressed.
Main takeaways
Blood pressure monitoring
Self-monitoring and remote management are well accepted by patients and have clear and proven benefits for both professionals and patients.⁹ ¹⁰
Frequent self-monitoring by patients at home gives a better measure of underlying blood pressure and hypertension than clinical office blood pressure measurement.⁹
Remote titration of antihypertensives according to a predefined plan decreases professional workload and is both effective and cost-effective.¹³
Changes during pregnancy require careful monitoring of the blood pressure to ensure the safety of both the mother and child.¹⁵
ABPM is the golden standard for diagnosing hypertension. However, it has become less popular as it leads to decreased sleep quality during the night which can cause misleading readings.²



