Clinical Research & Literature — Cardiology
Blood Pressure
Elevated blood pressure can be easily detected through measuring, and can often be treated effectively with medications.

Clinical Research & Literature — Cardiology
Blood Pressure
Elevated blood pressure can be easily detected through measuring, and can often be treated effectively with medications.
Hypertension
Hypertension, also known as high or raised blood pressure, is a condition in which the blood vessels have persistently raised pressure. It is a major cause of premature death worldwide, with 1 in 4 men and 1 in 5 women – over a billion people – having the condition. The number of adults aged 30–79 years with hypertension has increased from 650 million to 1.28 billion in the last thirty years of which nearly half did not know they had hypertension. Hypertension significantly increases the risk of heart, brain, and kidney diseases, and is one of the top causes of death and disease throughout the world as addressed in the cardiorenal continuum. It can be easily detected through measuring blood pressure, at home or in a health centre, and can often be treated effectively with medications that are low cost.¹
2018 ESC/ESH Guidelines for the management of arterial hypertension²
Several proven, highly effective, and well-tolerated lifestyle and drug treatment strategies can achieve reduction in Blood Pressure (BP). Despite this, BP control rates remain poor worldwide and are far from satisfactory across Europe. Consequently, hypertension remains the major preventable cause of cardiovascular disease (CVD) and all-cause death globally. These guidelines summarize and evaluate available evidence with the aim of assisting health professionals in selecting the best strategy.
Secondary hypertension³
Secondary hypertension is elevated blood pressure (BP), which is secondary to an identifiable cause. Since its prevalence is relatively low, performing routine evaluations in every case of hypertension is not cost-effective and is also time-consuming. This paper summarizes the various causes of secondary hypertension, various treatments, and management options. Furthermore, available evidence about the best management strategies for an individual patient with a given condition will be covered, to help health care professionals to implement the right management strategy.
Cardiorenal Continuum⁴
Cardiovascular events rarely occur in patients without underlying disease; rather, they typically take place at the final stage of a pathophysiological process that results in progressive vascular damage, including vital organ damage—specifically, the kidney and the heart. Renal and cardiovascular diseases share the same enteropathogenic risk factors. If these factors are controlled, then atherosclerotic process evolution and further target-organ damage or cardiovascular events can be prevented.
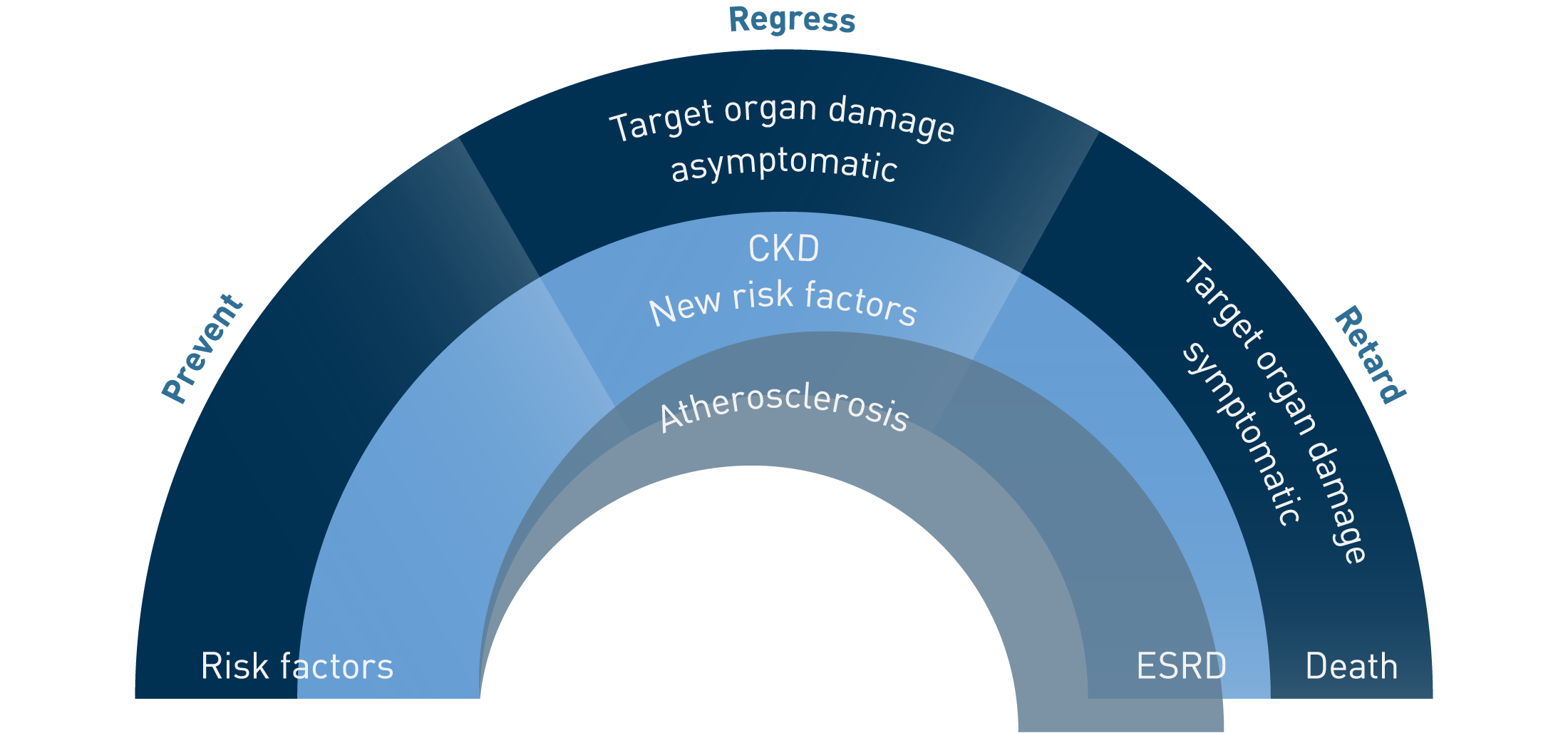
Graphic representation of the cardiorenal continuum.
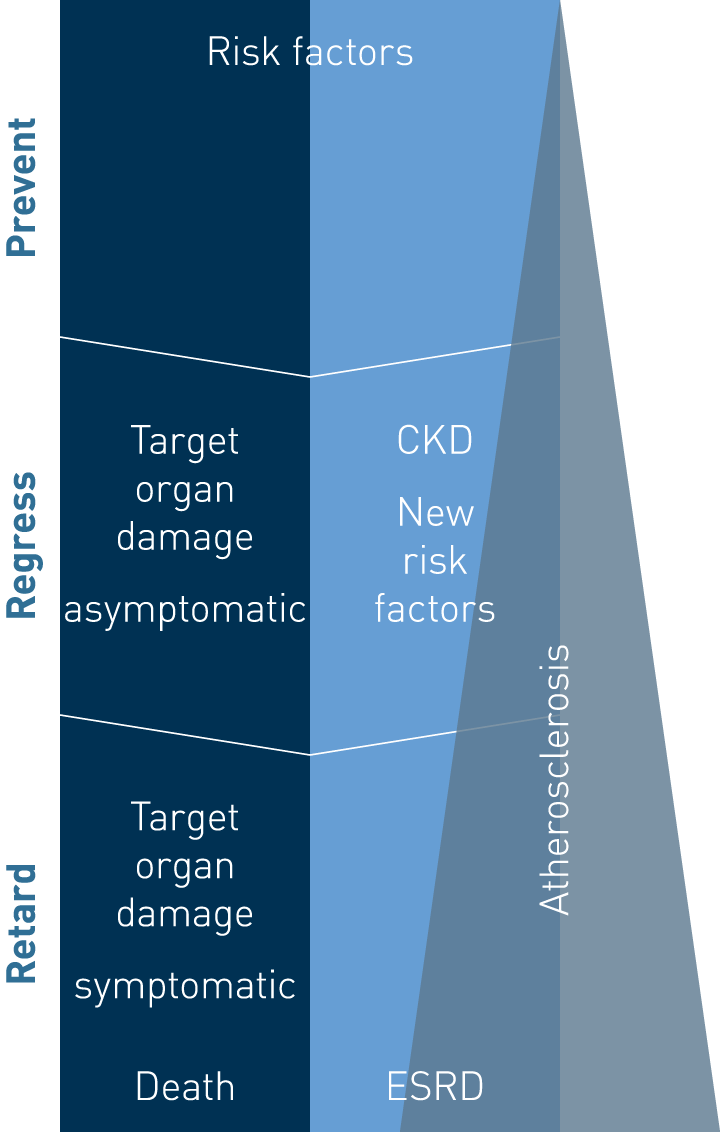
Graphic representation of the cardiorenal continuum.
Nocturnal blood pressure
Nocturnal hypertension is the most prevalent phenotype of masked hypertension and more than one-third of the individuals with nocturnal hypertension had normal ABPM during daytime activities, namely Isolated Nocturnal Hypertension⁵
Prevalence of isolated nocturnal hypertension according to 2018 European Society of Cardiology and European Society of Hypertension office blood pressure categories⁶
Isolated nocturnal hypertension is a specific subtype of nocturnal hypertension which is characterized by elevated blood pressure at night with normal daytime blood pressure. Individuals with isolated nocturnal hypertension may experience more arterial stiffness, cardiac damage, and a higher risk of cardiovascular events and death. A recent study also showed that this condition could be an early manifestation of hypertensive disease. This paper studies the prevalence of isolated nocturnal hypertension and its relationship with office blood pressure categories defined by 2018 European Society of Cardiology and European Society of Hypertension (ESC/ESH) guidelines.
Isolated Nocturnal Hypertension: What Do We Know and What Can We Do?⁷
Blood pressure monitoring and studies have increased the awareness of nocturnal hypertension and its influence on target organ damage. Nocturnal hypertension is associated with an inadequate drop or even an increase in blood pressure at night compared to daytime blood pressure. Investigations have concluded that inadequate drop or reverse dipping is a predictor of cardiovascular events independently of circadian blood pressure patterns. This paper discusses the mechanisms, diagnosis, and treatment of nocturnal hypertension and why the timing of drug administration plays a crucial role in reducing nighttime blood pressure.
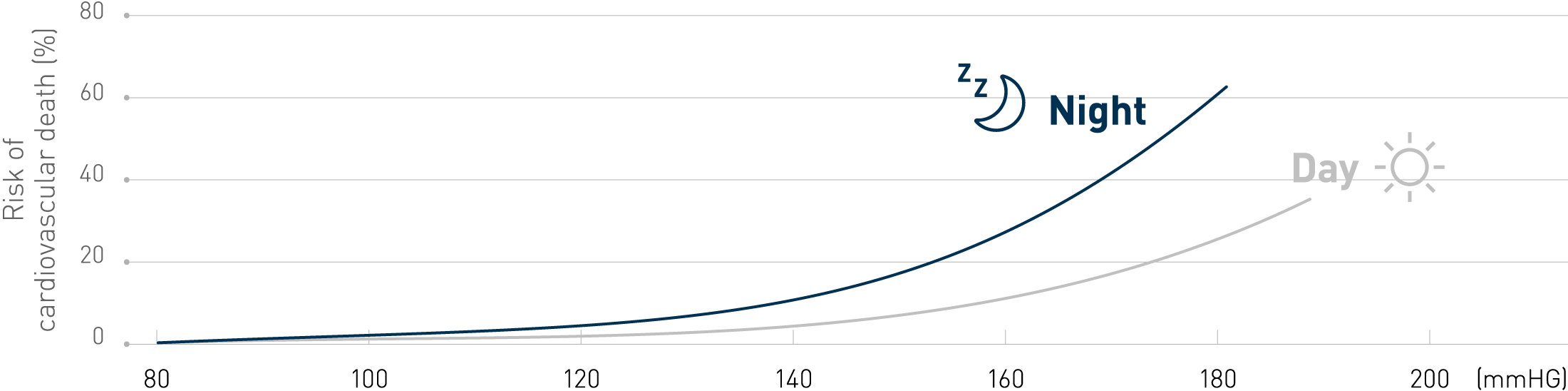
Nighttime blood pressure values and non-dipping patters are stronger predictors of cardiovascular outcomes than daytime values⁷
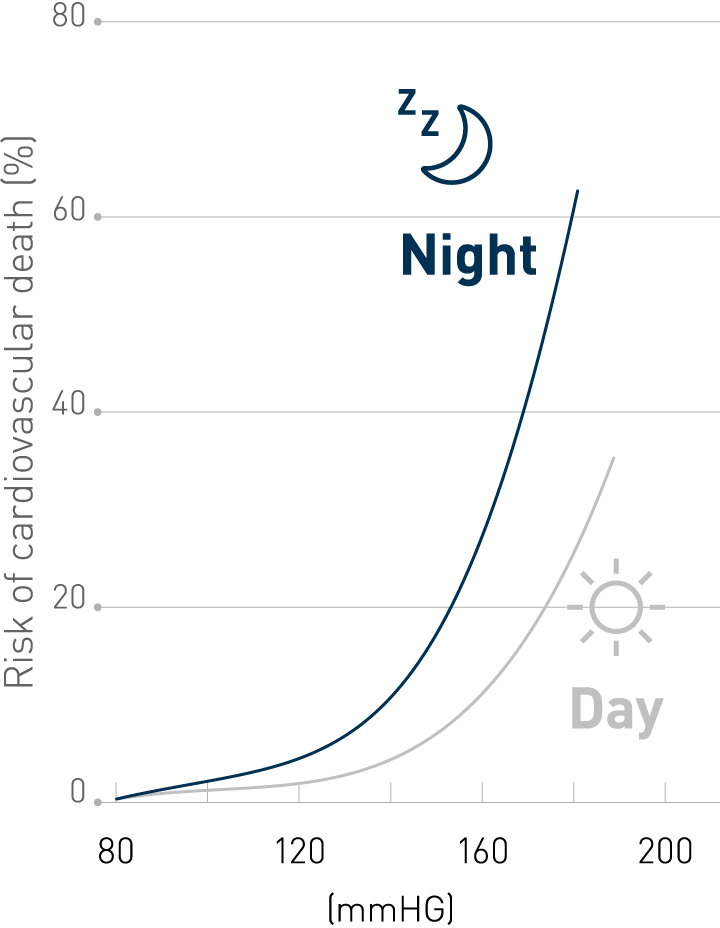
Nighttime blood pressure values and non-dipping patters are stronger predictors of cardiovascular outcomes than daytime values⁷
The Role of Nocturnal Blood Pressure and Sleep Quality in Hypertension Management⁸
Hypertension and the prevention of its associated cardiovascular risks can be managed by an accurate measurement, prediction, and treatment of high blood pressure during the day. However, nocturnal blood pressure can still increase the risk of fatal and non-fatal cardiovascular events. Nighttime blood pressure is usually evaluated with an ambulatory blood pressure monitoring device, however, the availability is low and it can cause sleep disturbances. Home blood pressure monitoring can be an alternative and is more preferred by patients. The NightView is a new validated blood pressure device which offers the possibility to measure daytime and nighttime blood pressure with minimal sleep disturbance.
Development and evaluation of a home nocturnal blood pressure monitoring system using a wrist-cuff device⁹
The conventional nocturnal blood pressure monitoring (NBPM) systems can disturb sleep and lead to false measurements. The present study compared the validity and acceptability of a newly developed wrist-cuff system with that of the conventional upper arm-cuff system for NBPM. Compared with the arm-cuff system, the wrist-cuff system had significantly lower systolic BP. Furthermore, sleep disturbance during NBPM was reported in less than 20% with the wrist-cuff system and in 70% with the arm-cuff system. A significantly higher rate of participants who wore the wrist-cuff system reported that they were not bothered by various stimuli, such as noise, during NBPM.
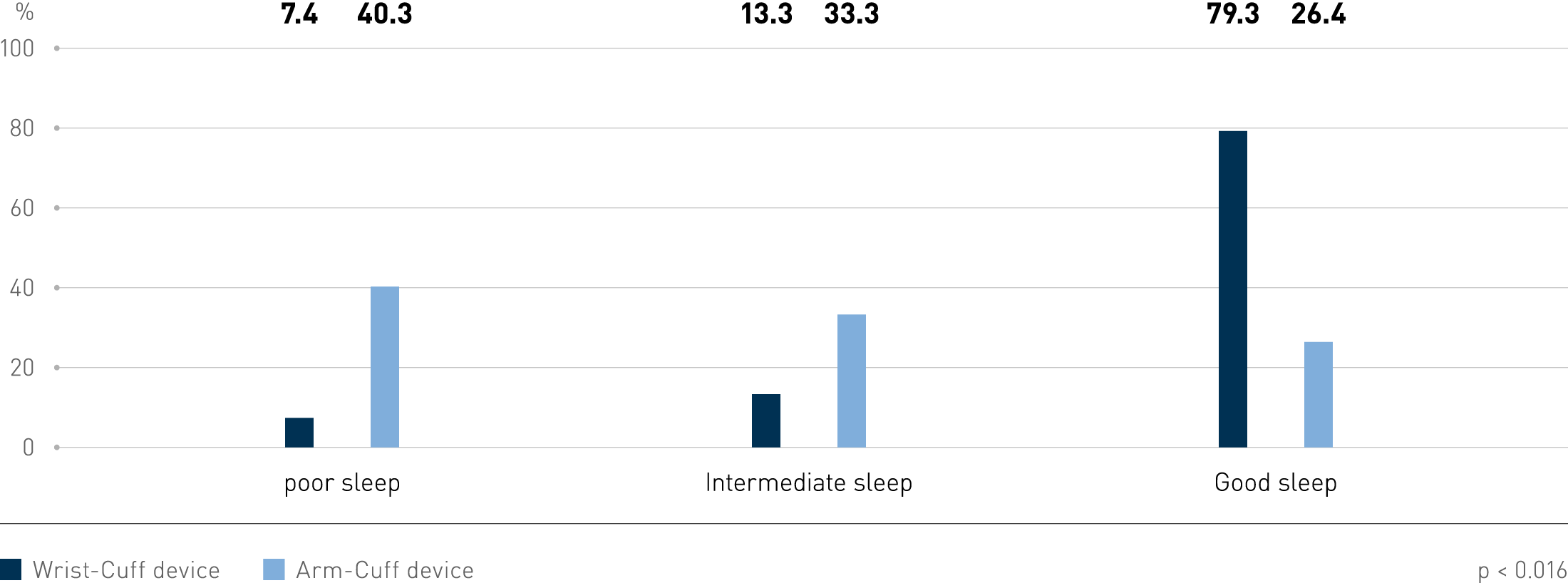
Comparison of the quality of sleep during nocturnal blood pressure monitoring between wrist-cuff and arm-cuff system⁸
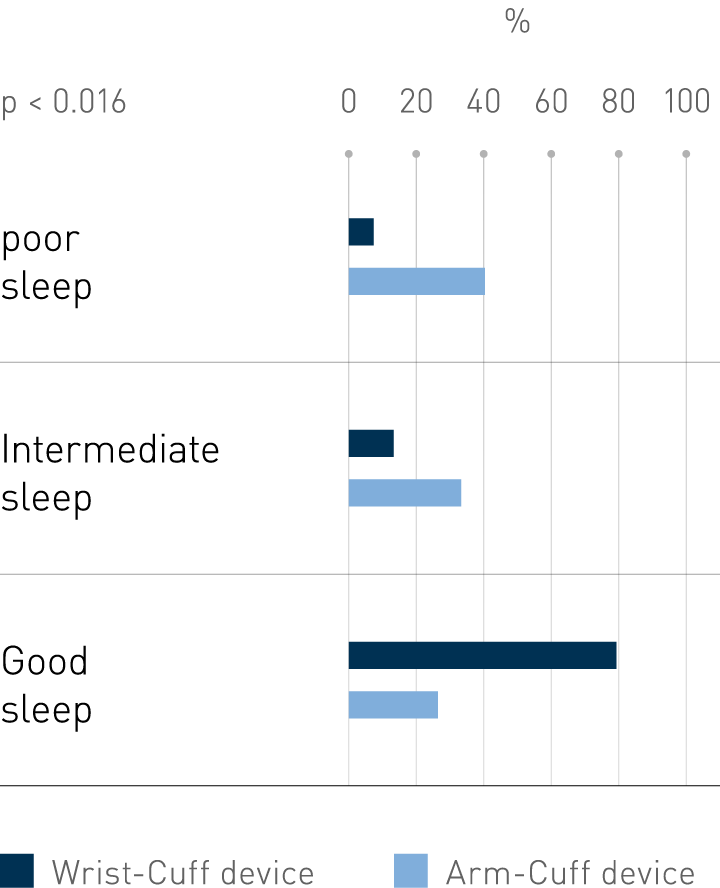
Comparison of the quality of sleep during nocturnal blood pressure monitoring between wrist-cuff and arm-cuff system⁸
Main takeaways
Blood pressure
Hypertension significantly increases the risk of heart, brain, and kidney diseases, and is one of the top causes of death and disease throughout the world.¹
Nocturnal hypertension is the most prevalent phenotype of masked hypertension.⁵
Nocturnal hypertension is a better predictor for cardiovascular events.⁶
The management of hypertension should direct towards controlling blood pressure for 24 hours, including nocturnal and morning periods.⁹
The golden standard to measure nocturnal blood pressure is ABPM, but the use of connected home blood pressure monitors could prove to be more feasible for the assessment of nocturnal blood pressure.⁸



